Global Health and Education


Circulatory System: Blood Flow Pathway Through the Heart
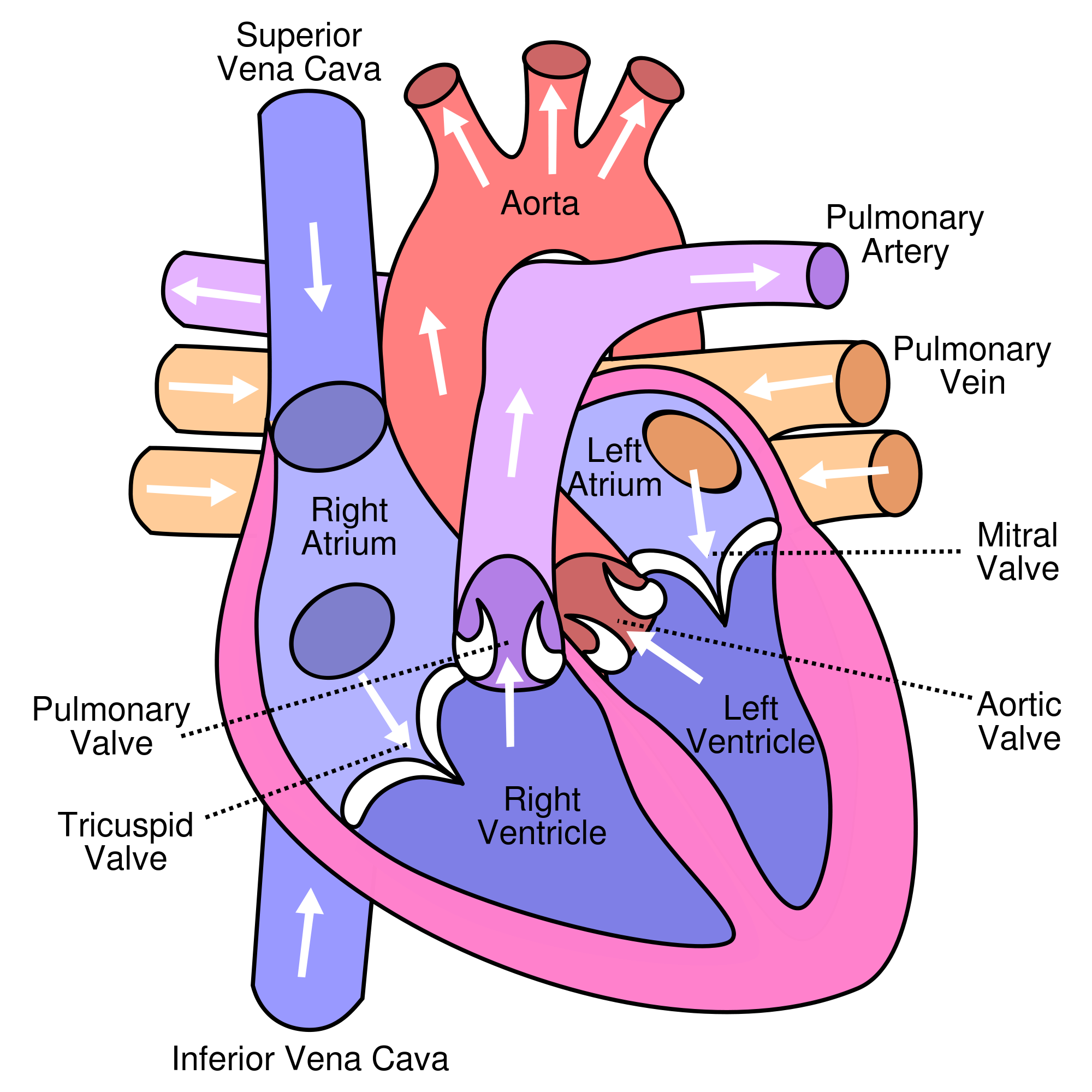
Pathway of blood through the heart.
In this educational lesson, we learn about the blood flow order through the human heart in 14 easy steps , from the superior and inferior vena cava to the atria and ventricles. Come also learn with us the heart’s anatomy, including where deoxygenated and oxygenated blood flow, in the superior vena cava, inferior vena cava, atrium, ventricle, aorta, pulmonary arteries, pulmonary veins, and coronary arteries.
Quick & Easy Video on Blood Flow Pathway Through the Heart
Blood flow order: step by step animation tutorial.
To gain a visual step-by-step understanding, check out our quick and easy video on the blood flow pathway through the heart in less than 90 seconds. Please notice that blue represents deoxygenated blood , and red represents oxygenated blood .
14 Steps of Blood Flow Through the Heart
In summary from the video, in 14 steps, blood flows through the heart in the following order: 1) body –> 2) inferior/superior vena cava –> 3) right atrium –> 4) tricuspid valve –> 5) right ventricle –> 6) pulmonary arteries –> 7) lu ngs –> 8) pulmonary veins –> 9) left atrium –> 10) mitral or bicuspid valve –> 11) left ventricle –> 12) aortic valve –> 13) aorta –> 14) body .

Superior Vena Cava & Inferior Vena Cava
The vena cava is the largest vein in the body that delivers oxygen-poor or deoxygenated blood to the right atrium of the heart. The superior vena cava comes from the upper part of the body, including the brain and arms, while the inferior vena cava comes from the abdominal area and legs.
Left Atrium & Right Atrium
The atria are the top two chambers of the heart that receive incoming blood from the body. The right atrium receives deoxygenated blood through the superior and inferior vena cavas from the body and pumps it to the right ventricle through the tricuspid valve, which opens to allow the blood flow through and closes to prevent blood backing up the atrium. The left atrium receives oxygenated blood through the pulmonary veins from the lungs. It pumps the blood through the mitral valve to the left ventricle. Attached to the atria are the pouches called auricles that expand to allow the atria to include more blood volume. For fetal circulation , there is a special hole shunt between the left atrium and right atrium called the foramen ovale that diverts blood away from the lungs and goes directly to the rest of the fetus’s body.
Left Ventricle & Right Ventricle
The ventricles are the two lower chambers of the heart. The right ventricle receives oxygen-poor blood from the right atrium and pumps it through the pulmonic semilunar valve to the pulmonary artery and into the lungs to be filled with oxygen. On the other hand, the left ventricle receives oxygen-rich blood from the left atrium and pumps it through the aortic semilunar valve to the aorta to deliver the oxygen to the rest of the body.
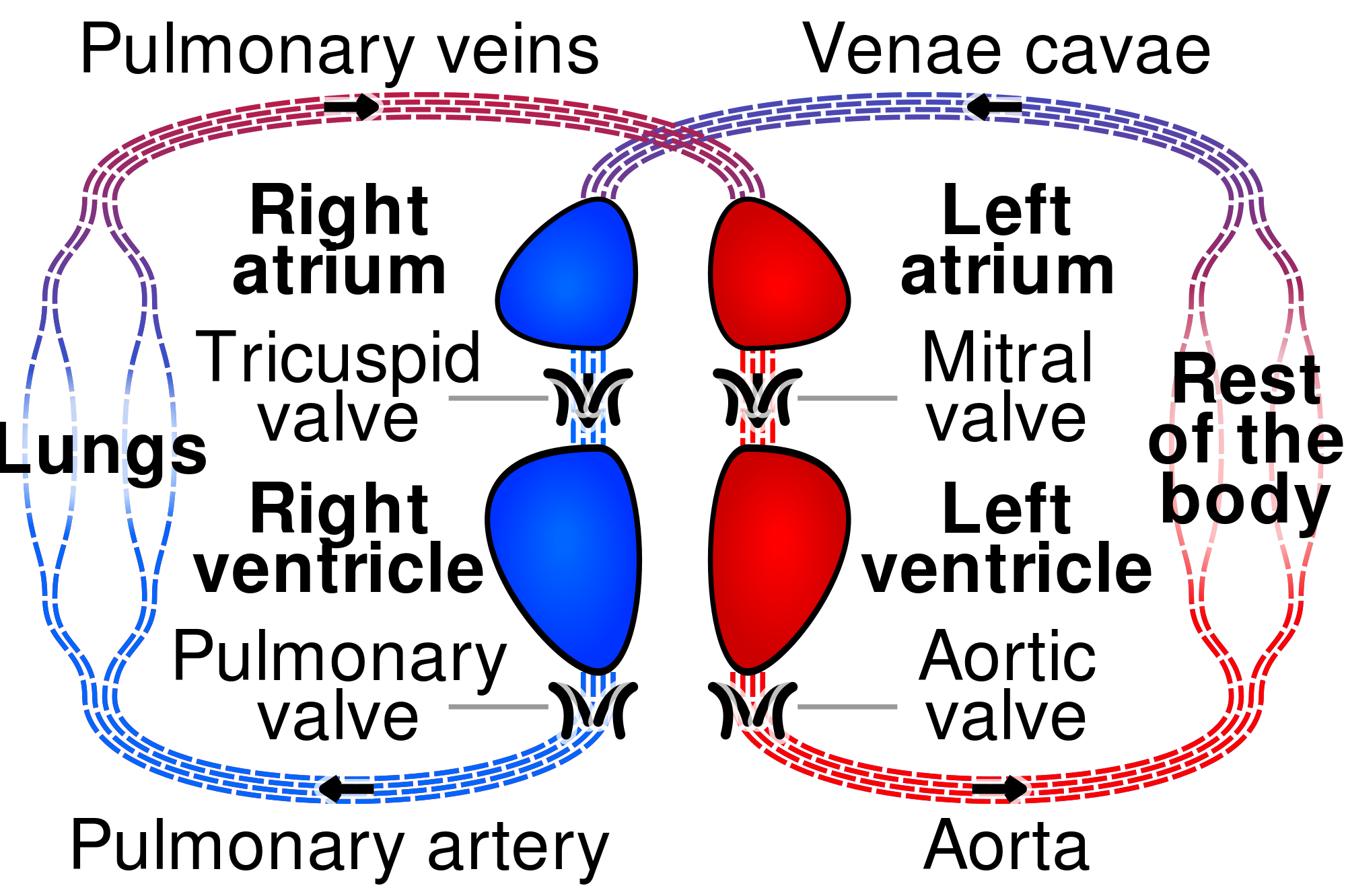
Pulmonary Arteries & Pulmonary Veins
The pulmonary arteries deliver oxygen-poor blood from the right ventricle of the heart to the lungs, while the pulmonary veins deliver oxygen-rich blood from the lungs to the left atrium of the heart. For fetal circulation , there is a special hole shunt called the ductus arteriosus that is between the pulmonary arteries and aorta to divert blood away from the fetus’s lungs. Learn more about how the ductus arteriosus works here, and why it’s there for fetuses .
Aorta & Coronary Arteries
The aorta is the largest artery in the body that leads from the left ventricle of the heart to the rest of the body. It carries oxygen-rich blood to deliver to the body’s cells. As an artery, it contains thicker walls than veins because it has to withstand the tough pumping blood pressure of the heart.
The coronary arteries are a set of arteries that branch off the aorta and are located on the heart. They carry oxygenated blood and nutrients to nourish the heart tissue cells. When the coronary arteries are clogged by excessive fatty tissue in cholesterol, it can lead to a lack of nutrients and oxygen for the heart, whose cells begin to perish, and this leads to a heart attack.
Final Test Your Knowledge! 😀
Summary: what are the 14 steps of blood flow through the heart.
Blood flows through the heart in the following order: 1) body –> 2) inferior/superior vena cava –> 3) right atrium –> 4) tricuspid valve –> 5) right ventricle –> 6) pulmonary arteries –> 7) lu ngs –> 8) pulmonary veins –> 9) left atrium –> 10) mitral or bicuspid valve –> 11) left ventricle –> 12) aortic valve –> 13) aorta –> 14) body .
Big thank you to our kind supporters! Please Like and Subscribe to our Email List at moosmosis.org , Facebook , Twitter , Youtube to support our open-access youth education initiatives! 🙂
Copyright © 2022 Moosmosis Organization: All Rights Reserved
All rights reserved. This essay or any portion thereof may not be reproduced or used in any manner whatsoever without the express written permission of the publisher.

Please Like and Subscribe to our Email List at moosmosis.org , Facebook , Twitter , Youtube to support our open-access youth education initiatives! 🙂
*This article has been accepted into Moosmosis’s Journal of Global Health and Education . Accepted 2020. Published July 2020.
Works cited.
- Tubbs RS. The heart is simply a muscle. Clin Anat . 2016;29(3):267-268. doi:10.1002/ca.22704
- Miao JH, Makaryus AN. Anatomy, Thorax, Heart Veins. In: StatPearls . Treasure Island (FL): StatPearls Publishing; 2020.
- Anderson RH, Wilcox BR. Understanding cardiac anatomy: the prerequisite for optimal cardiac surgery. Ann Thorac Surg . 1995;59(6):1366-1375. doi:10.1016/0003-4975(95)00195-q
- Courchaine K, Rykiel G, Rugonyi S. Influence of blood flow on cardiac development. Prog Biophys Mol Biol . 2018;137:95-110. doi:10.1016/j.pbiomolbio.2018.05.005
- Efimov IR. Innovation in optical imaging: looking inside the heart. Heart Rhythm . 2007;4(7):925-926. doi:10.1016/j.hrthm.2007.04.006
Do you “LUB” our hearty content? Please share, subscribe, & like for more! 😀
Share this:.

- Share on Tumblr
Categories: Biology , stem
Tagged as: anatomy , Biology , blood flow , cardiovascular system , circulatory system , college , education , Feature , featured , heart , Journal of Global Health and Education , life , medicine , physiology , school , science , university
Published by Moosmosis
Passionate about lifelong learning, global health, and education! Check out our Moosmosis team's award-winning youth education site and articles @moosmosis.org Recognized by United Nations Academic Impact. View all posts by Moosmosis
250 replies »
- Pingback: Medical School: Learning Pain Management for Medical Students – Moosmosis
Good and Simple learning
Like Liked by 1 person
Thank you Vivek! Happy learning! 🙂
- Pingback: Epidural Hematoma vs Subdural Hematoma vs Subarachnoid Hemorrhage: Symptoms, Diagnosis, Treatment, and Prognosis – Moosmosis
- Pingback: Heart Block: First Degree vs Second Degree (Type I and Type 2) vs Third Degree – ECG Findings, Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Aortic Stenosis vs Aortic Regurgitation: Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
Wonderful diagrams and article on heart blood flow! Wholesome and helpful ❤️
Thank you so much Kay! Have a wonderful day ❤️
Good job done keep it up✌🏻
Thank you so much!!!
Thanks a lot of 👍
Like Liked by 2 people
- Pingback: Systolic Heart Failure vs Diastolic Heart Failure: Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Stanford Type A vs Stanford Type B Aortic Dissection: Anatomy, Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Heart Attack versus Heart Failure: Anatomy, Symptoms, Diagnosis, Treatment, and Prognosis [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Sleeve Gastrectomy vs Roux-en-Y Gastric Bypass vs Adjustable Gastric Banding: Anatomy, Mechanisms, Treatment, and Prognosis – Moosmosis
Excellent and extremely helpful! I was super confused about the order, this helped me understand the heart blood flow steps so much better, thanks!!
Thank you so much Jackie! Happy to help!
- Pingback: Comparing and Contrasting Acute Cholecystitis vs. Acute Cholangitis: Symptoms, Causes, Treatments, and Prognosis – Moosmosis
- Pingback: Biology Major vs Chemistry Major vs Biochemistry Major in College – Moosmosis
Very high level and comprehensive post! Thanks for visiting my blog. I can’t use the “like” buttons on your blog.
Thank you so much! You have a great blog too! Have a nice day!
- Pingback: The Modified Barium Swallow Study: Exploring Anatomy, Procedure, Diagnoses, and Medical Findings – Moosmosis
- Pingback: Top 70 Medical Abbreviations in Medical Record Notes and Sample History & Physical Exam Note – Moosmosis
- Pingback: Inflammatory Bowel Diseases – Crohn’s Disease vs. Ulcerative Colitis: Symptoms, Diagnosis, Treatments, and Prognosis – Moosmosis
Wonderful article on heart blood flow!
Thank you so much for your kind words, Susie!
- Pingback: Urinary Tract Infections (UTI) – Cystitis vs Pyelonephritis: Symptoms, Diagnosis, Treatments, and Prognosis – Moosmosis
This is so helpful! Made heart blood flow steps easy to understand, thanks!
You’re very welcome! So glad you found it helpful
- Pingback: Types of Femoral Fractures: Femoral Head, Neck, Shaft, and Distal Femoral Fractures -Anatomy, Mechanisms, Treatment, and Prognosis – Moosmosis
- Pingback: Happy New Year and New Year Resolutions: 25 Health and Wellness Tips for a Healthier and Happier New Year – Moosmosis
Amazing! Excellent article on heart blood flow steps.
Thank you so much! Have an excellent day!! 😄
Excellent! So helpful
Thank you so much! We’re happy you found it helpful! ❤️❤️❤️
Thank you!! We love you too dear reader!! ❤️❤️❤️
Thanks for signing on to my blog – as an instructor in anatomy and physiology for medical students I think this blog is very helpful!
Thank you so much!!! ❤️ Your blog is very helpful and wonderful too! We hope you have a great day!
- Pingback: Circulatory System 101: Advantages and Disadvantages of Cardiac MRI versus Cardiac CT [MCAT, USMLE, Biology, Medicine] – Moosmosis
- Pingback: Types of Stroke – Ischemic Stroke vs Hemorrhagic Stroke: Symptoms, Diagnosis, Treatment, and Prognosis – Moosmosis
- Pingback: NBME Internal Medicine Form 6: Notes and Explanations for the Answers – Moosmosis
- Pingback: Top 25 Nutritious Foods to Eat for Health, Energy, and Wellness – Moosmosis
- Pingback: NBME Internal Medicine Form 4: Notes and Explanations for the Answers – Moosmosis
- Pingback: Top 20 Super Foods to Eat for a Healthy Long Life – Moosmosis
- Pingback: Top 20 Health and Wellness Tips for Successful Weight Loss and a Healthy Lifestyle – Moosmosis
- Pingback: NBME Internal Medicine Form 5: Notes and Explanations for the Answers – Moosmosis
- Pingback: Fueling Vitality: Top 25 Foods for Energy, Mood Boosting, and Happiness – Moosmosis
- Pingback: Pericarditis vs Cardiac Tamponade: Symptoms, Diagnosis, Treatment, and Prognosis – Moosmosis
Leave a comment Cancel reply
Thank you for visiting.
- 2,678,465 Lifelong Learners!
Join Moosmosis and our wonderful lifelong learning community today! Free lessons and student opportunities
Email Address:
Subscribe for Free!
Today’s Top Posts

Our Community
Choose a Language
Please Like to Support!
- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
Circulation Station
Put your fingers on your wrist. Feel something throbbing just below the surface of your skin? It’s your pulse, letting you know that your heart is working hard. Each time your heart beats, it pumps blood along a network of tubes called blood vessels. This network, along with your heart, is known as the circulatory system, and it reaches every cell in your body. Your blood travels in a never-ending cycle, delivering supplies and taking away wastes. Within your blood, red blood cells have a specialized task. They pick up oxygen in your lungs and carry it to your body’s tissues and organs. Your blood then transports carbon dioxide back to the lungs where you can breathe it out.
- Heart Blood circulation begins in the heart.
- Lungs Red blood cells pick up oxygen in the lungs.
- Arteries Blood travels away from the heart and lungs through the arteries ( ar -tuh-reez).
- Capillaries Red blood cells drop off oxygen to the cells through tiny tubes called capillaries ( cap -ill-air-ies).
- Veins Blood then returns to the heart through the veins (vayns) and the cycle begins again.
The Body’s Superhighway
Welcome to the hardest working muscle in your body. Your heart powers the circulatory system. Think of your heart as two pumps, working side by side. One pump receives oxygen-poor blood from your body and pushes it next door to your lungs where it picks up oxygen. The other pump receives oxygen-rich blood back from your lungs and gives it a boost out to your body.
- Right atrium, Left atrium The right atrium (ay-tree-um) receives blood that needs to go to the lungs while the left atrium receives blood ready to go out to the body. Together, these pumps are called the atria ( ay -tree-uh).
- Valves When these valves open, blood is pumped from the two atria ( ay -tree-uh), to the ventricles below.
- Right ventricle, Left ventricle The right ventricle ( ven -trick-ul) pumps oxygen-poor blood to the lungs. At the same time, the left ventricle pumps oxygen-rich blood out to the body.
- Valves These valves open to let the ventricles, ( ven -trick-ulz), pump blood out to the lungs and body.
Your lungs are specially equipped to do a very important job. Take a deep breath. Your spongy lungs have just filled with air and allowed oxygen to pass into your blood. Now breathe out. Your lungs have worked again—this time letting gasses you don’t need, like carbon dioxide, pass from your blood back out into the air.
- Trachea The trachea ( tray -kee-uh) is the windpipe that you breathe through.
- Bronchi The bronchi ( bron -keye) are tubes that transport air from the trachea to each lung. They extend like tree branches into the lung.
- Bronchioles The bronchioles ( bron -kee-oles) branch out from the bronchi into even smaller tubes.
- Alveoli The alveoli (al- vee -oh-lie) are tiny air sacs at the end of the bronchioles (bron-kee-oles). Red blood cells drop off carbon dioxide and pick up fresh oxygen here.
Your arteries ( ar -tuh-reez) are blood vessels that carry oxygen-rich blood from your heart out to the rest of your body. These muscular tubes have thick strong walls to handle the high pressure of freshly pumped blood. In illustrations arteries are usually colored red because the blood inside of them is bright red—a sign that red blood cells are carrying lots of oxygen.
- Muscle Muscle is built into the artery wall.
Capillaries
Your capillaries ( cap -ill-air-ies) are tiny blood vessels that distribute blood from your arteries ( ar -tuh-reez) to the billions of cells in your body, and then to your veins (vayns). The walls of capillaries are very thin—so thin that nutrients and oxygen can pass right through them. As red blood cells pass through the capillaries, they drop off the oxygen that your cells need to live, and pick up the waste gas, carbon dioxide.
- Capillary wall Capillary ( cap -ill-air-e) walls are only a single cell thick.
Veins (vayns) are blood vessels that carry your oxygen-poor blood back to the heart. This is a pretty difficult job. When blood flows to your toes, it’s a downhill ride. Getting the blood back up to your heart is a little harder. The veins in your arms and legs have little flap-like valves that help prevent blood from flowing backwards.
- Muscle The muscle in the vein wall is much thinner than the muscle in the artery (ar-tuh-re) wall.
- Valve Veins (vayns) in the arms and legs have valves that help blood to keep moving forward.
Complete the Loop
Around and Around We Go Your blood circulates around your body more than a thousand times a day. Imagine for a moment that you are a red blood cell. See if you can complete the tasks below.
Task: You are a red blood cell and have just arrived at the heart. Where do you go to pick up oxygen?
Task: You are in the lungs and have just loaded up with oxygen. Where do you go next?
Task: The heart is ready to pump you out to tissues and organs that need the oxygen you are carrying. Do you travel through an artery or vein?
Task: You need to deliver oxygen to the organ that does your thinking. Where do you go?
Task: You have delivered oxygen to the brain and have picked up the waste gas, carbon dioxide. You are ready to drop off your carbon dioxide and pick up some more fresh oxygen. Do you travel through an artery or vein?
A Doctor Making a Difference
Helen Brooke Taussig was a frail child who suffered from the learning problem, dyslexia (dis- lex -ee-uh). When she grew older, she also lost her hearing. Nevertheless, she beat the odds to become a doctor and make an important medical discovery. Dr. Taussig worked with “blue babies,” whose color at birth indicated that they were not getting enough oxygen. Some of these babies died immediately. Others only lived a few years.
Dr. Taussig discovered that these babies had poor blood flow between their hearts and lungs. She worked with Dr. Alfred Blalock and his brilliant technician, Vivien Thomas, and developed a new heart operation for “blue babies.” In 1944 they had their first success. Since then, the lives of many children have been saved.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Order of Blood Flow Through the Heart
Mapping the Route Through the Body's Circulatory System
- Heart Anatomy
- Blood Flow Through the Heart
- Blood Flow Through the Body
- Role of Heart Valves
- Adverse Conditions
Blood flow through the heart involves contractions of the heart muscle to move blood from the right chambers of the heart to the lungs —where it receives oxygen—and then to the left chambers of the heart where it is pumped to the rest of the body through a network of blood vessels.
Involved in this process are four heart valves that are synchronized to open and shut with each heartbeat. This ensures the consistent flow of blood in one direction from the heart via arteries (which carry oxygenated blood) and back to the heart via veins (which carry deoxygenated blood along with carbon dioxide).
This article maps the order of blood flow through the heart. It also describes problems that can affect blood flow when different parts of the circulatory system malfunction.
Components of the Heart Involved in Blood Flow
The heart has two upper chambers, called the left and right atriums , and two lower chambers, called the left and right ventricles . With each heartbeat, blood moves from one chamber to the next through a series of heart valves.
The heart rate and rhythm are controlled by the cardiac conduction system which delivers electric impulses that contract and relax the heart muscle.
Several major arteries and veins are involved in this process:
- The pulmonary artery transfers blood from the heart to the lungs.
- The pulmonary vein transfers blood from the lungs to the heart.
- The aorta delivers oxygenated blood from the heart to the rest of the body.
- The superior vena cava and inferior vena cava transport deoxygenated blood from the body back to the heart.
There are four valves that control blood flow in and out of the chambers of the heart:
- The tricuspid valve is located between the right atrium and the right ventricle.
- The pulmonary valve is located between the right ventricle and the pulmonary artery.
- The mitral valve is located between the left atrium and the left ventricle.
- The aortic valve is located between the left ventricle and the aorta.
Order of Blood Flow Through the Heart: Step by Step
Right side of heart.
Here is the path that blood takes in the right side of the heart:
- The blood first enters the right atrium from the superior and inferior vena cava.
- It then flows through the tricuspid valve into the right ventricle.
- The blood then moves through the pulmonary valve into the pulmonary artery.
- The pulmonary artery carries blood to the lungs where it takes up oxygen.
Left Side of Heart
- Oxygenated blood returns to the heart through the pulmonary vein into the left atrium.
- The blood then moves through the mitral valve into the left ventricle.
- The left ventricle then pumps the blood through the aortic valve into the aorta.
- From the aorta, the blood is transported through the network of blood vessels, delivering oxygen and nutrients to tissues and taking carbon dioxide and wastes from tissues.
- Deoxygenated blood returns to the heart via the superior and inferior vena cava, and the cycle begins again.
Order of Blood Flow Through the Body: Step by Step
Once oxygenated blood leaves the heart, it is pumped through a network of vessels throughout the body to deliver nutrients and oxygen to cells.
Here is the path blood flows once it exits the left side of the heart:
- Oxygenated blood from the left side of the heart gets pumped out of the aorta, the largest vessel of the body. The aorta extends from the left ventricle of the heart down into the abdomen.
- Blood then flows through arteries that branch off from the aorta. These arteries deliver blood to different areas of the body.
- Arteries then split into smaller vessels known as arterioles, which then carry blood to the smallest vessels in the body—the capillaries.
- The capillaries deliver oxygen and nutrients to the tissues of your body and simultaneously remove carbon dioxide to be eliminated in the lungs.
- Deoxygenated blood from the capillaries then flows back to the heart through small vessels known as venules.
- The venules then gradually merge to form veins.
- Blood enters back into the heart via large veins known as the superior and inferior vena cava.
- Blood is then pumped through the right side of the heart, into the lungs to get oxygen, and back into the left side of the heart.
What Is the Correct Order of Blood Vessels From the Heart?
Oxygenated blood from the left side of the heart gets pumped out of the aorta. From there, blood flows through arteries, arterioles, and then capillaries (tiny blood vessels that transport blood, nutrients, and oxygen to cells).
Deoxygenated blood from the capillaries then flows back to the heart through venules, veins, and ultimately through the superior and inferior vena cava.
Role of Heart Valves With Blood Flow
The four heart valves prevent the backward flow of blood and keep blood moving in one direction. The valves are comprised of flaps of muscular tissues that open in one direction. The tricuspid, pulmonary, and aortic valves have three flaps, while the mitral valve has two flaps.
The tricuspid and mitral valves are located on each end of the two ventricles. They act as one-way inlets of blood on one side of a ventricle and one-way outlets of blood on the other side of a ventricle.
The pulmonary valve regulates the flow of blood in and out of the lungs, while the aortic valve regulates the flow of blood out of the heart and to the body.
The sound of your heartbeat is largely due to the opening and shutting of the valves. The low-pitched "lub" sound is due to the shutting of mitral and tricuspid valves, while the high-pitched "dub" sound is caused by the shutting of the aortic and pulmonary valves.
Conditions That Affect Normal Blood Flow
A healthy heart normally beats anywhere from 60 to 70 times per minute when you're at rest. This rate can be higher or lower depending on your general health and physical fitness. Athletes generally have a lower resting heart rate.
Your heart rate will increase when you move or engage in physical activity. This is because your muscles use oxygen while they work. In response, the heart works harder to bring oxygenated blood where it is needed.
Certain conditions can affect blood flow to and from the heart, including:
- Cardiac arrhythmia : This is a group of disorders that cause irregular heartbeats due to problems with electrical impulses. Atrial fibrillation is a common form of this.
- Heart blocks : These are problems with the cardiac conduction system. Two main types are an atrioventricular (AV) block and a bundle branch block .
- Heart valve disease : Damaged valves can leak and reduce the amount of blood delivered to tissues. The cause may be congenital (something you are born with), degenerative (in which a valve gradually wears out with age), or due to heart disease.
- Heart failure : This is when the heart is unable to pump enough blood to meet the body's needs. The causes are many, including heart disease, lung disease, genetics, and infections.
- Cardiac ischemia : This is reduced blood flow due to a partially or fully obstructed blood vessel. One common cause of this is a heart attack.
Blood flow moves in one direction through the chambers of the heart. Electrical impulses are generated to make your heart beat. Heart valves open and shut to regulate blood flow. Cardiac arrhythmia, heart blocks, heart valve disease, heart failure, and cardiac ischemia can all affect the normal flow of blood to and from the heart.
National Heart, Lung, and Blood Institute. How the heart works .
National Heart, Lung, and Blood Institute. Conduction disorders .
NHS Inform. How the heart works .
American Heart Association. About heart valves .
Centers for Disease Control and Prevention. Valvular heart disease .
Skrzynia C, Berg JS, Willis MS, Jensen BC. Genetics and heart failure: a concise guide for the clinician . Curr Cardiol Rev . 2015;11(1):10-7. doi:10.2174/1573403X09666131117170446
Centers for Disease Control and Prevention. How the heart works .
The Texas Heart Institute at St. Luke’s Episcopal Hospital. Heart Anatomy .
YourHeartValve.com/Edwards Lifesciences. Basic Anatomy and Function of the Heart .
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
Module 4: The Cardiovascular System: Blood Vessels and Circulation
Circulatory pathways, learning objectives.
By the end of this section, you will be able to:
- Identify the vessels through which blood travels within the pulmonary circuit, beginning from the right ventricle of the heart and ending at the left atrium
- Create a flow chart showing the major systemic arteries through which blood travels from the aorta and its major branches, to the most significant arteries feeding into the right and left upper and lower limbs
- Create a flow chart showing the major systemic veins through which blood travels from the feet to the right atrium of the heart
Virtually every cell, tissue, organ, and system in the body is impacted by the circulatory system. This includes the generalized and more specialized functions of transport of materials, capillary exchange, maintaining health by transporting white blood cells and various immunoglobulins (antibodies), hemostasis, regulation of body temperature, and helping to maintain acid-base balance. In addition to these shared functions, many systems enjoy a unique relationship with the circulatory system. Table 1 summarizes these relationships.
As you learn about the vessels of the systemic and pulmonary circuits, notice that many arteries and veins share the same names, parallel one another throughout the body, and are very similar on the right and left sides of the body. These pairs of vessels will be traced through only one side of the body. Where differences occur in branching patterns or when vessels are singular, this will be indicated. For example, you will find a pair of femoral arteries and a pair of femoral veins, with one vessel on each side of the body. In contrast, some vessels closer to the midline of the body, such as the aorta, are unique. Moreover, some superficial veins, such as the great saphenous vein in the femoral region, have no arterial counterpart.
Another phenomenon that can make the study of vessels challenging is that names of vessels can change with location. Like a street that changes name as it passes through an intersection, an artery or vein can change names as it passes an anatomical landmark. For example, the left subclavian artery becomes the axillary artery as it passes through the body wall and into the axillary region, and then becomes the brachial artery as it flows from the axillary region into the upper arm (or brachium). You will also find examples of anastomoses where two blood vessels that previously branched reconnect. Anastomoses are especially common in veins, where they help maintain blood flow even when one vessel is blocked or narrowed, although there are some important ones in the arteries supplying the brain.
As you read about circular pathways, notice that there is an occasional, very large artery referred to as a trunk , a term indicating that the vessel gives rise to several smaller arteries. For example, the celiac trunk gives rise to the left gastric, common hepatic, and splenic arteries.
As you study this section, imagine you are on a “Voyage of Discovery” similar to Lewis and Clark’s expedition in 1804–1806, which followed rivers and streams through unfamiliar territory, seeking a water route from the Atlantic to the Pacific Ocean. You might envision being inside a miniature boat, exploring the various branches of the circulatory system. This simple approach has proven effective for many students in mastering these major circulatory patterns. Another approach that works well for many students is to create simple line drawings similar to the ones provided, labeling each of the major vessels. It is beyond the scope of this text to name every vessel in the body. However, we will attempt to discuss the major pathways for blood and acquaint you with the major named arteries and veins in the body. Also, please keep in mind that individual variations in circulation patterns are not uncommon.
Pulmonary Circulation
Recall that blood returning from the systemic circuit enters the right atrium via the superior and inferior venae cavae and the coronary sinus, which drains the blood supply of the heart muscle. These vessels will be described more fully later in this section. This blood is relatively low in oxygen and relatively high in carbon dioxide, since much of the oxygen has been extracted for use by the tissues and the waste gas carbon dioxide was picked up to be transported to the lungs for elimination. From the right atrium, blood moves into the right ventricle, which pumps it to the lungs for gas exchange. This system of vessels is referred to as the pulmonary circuit .
The single vessel exiting the right ventricle is the pulmonary trunk . At the base of the pulmonary trunk is the pulmonary semilunar valve, which prevents backflow of blood into the right ventricle during ventricular diastole. As the pulmonary trunk reaches the superior surface of the heart, it curves posteriorly and rapidly bifurcates (divides) into two branches, a left and a right pulmonary artery . To prevent confusion between these vessels, it is important to refer to the vessel exiting the heart as the pulmonary trunk, rather than also calling it a pulmonary artery. The pulmonary arteries in turn branch many times within the lung, forming a series of smaller arteries and arterioles that eventually lead to the pulmonary capillaries. The pulmonary capillaries surround lung structures known as alveoli that are the sites of oxygen and carbon dioxide exchange.
Once gas exchange is completed, oxygenated blood flows from the pulmonary capillaries into a series of pulmonary venules that eventually lead to a series of larger pulmonary veins . Four pulmonary veins, two on the left and two on the right, return blood to the left atrium. At this point, the pulmonary circuit is complete. The image, and table below defines the major arteries and veins of the pulmonary circuit discussed in the text.

Figure 1. Blood exiting from the right ventricle flows into the pulmonary trunk, which bifurcates into the two pulmonary arteries. These vessels branch to supply blood to the pulmonary capillaries, where gas exchange occurs within the lung alveoli. Blood returns via the pulmonary veins to the left atrium.
Overview of Systemic Arteries
Blood relatively high in oxygen concentration is returned from the pulmonary circuit to the left atrium via the four pulmonary veins. From the left atrium, blood moves into the left ventricle, which pumps blood into the aorta. The aorta and its branches—the systemic arteries—send blood to virtually every organ of the body.

Figure 2. The major systemic arteries shown here deliver oxygenated blood throughout the body.
The aorta is the largest artery in the body. It arises from the left ventricle and eventually descends to the abdominal region, where it bifurcates at the level of the fourth lumbar vertebra into the two common iliac arteries. The aorta consists of the ascending aorta, the aortic arch, and the descending aorta, which passes through the diaphragm and a landmark that divides into the superior thoracic and inferior abdominal components. Arteries originating from the aorta ultimately distribute blood to virtually all tissues of the body. At the base of the aorta is the aortic semilunar valve that prevents backflow of blood into the left ventricle while the heart is relaxing. After exiting the heart, the ascending aorta moves in a superior direction for approximately 5 cm and ends at the sternal angle. Following this ascent, it reverses direction, forming a graceful arc to the left, called the aortic arch . The aortic arch descends toward the inferior portions of the body and ends at the level of the intervertebral disk between the fourth and fifth thoracic vertebrae. Beyond this point, the descending aorta continues close to the bodies of the vertebrae and passes through an opening in the diaphragm known as the aortic hiatus . Superior to the diaphragm, the aorta is called the thoracic aorta , and inferior to the diaphragm, it is called the abdominal aorta . The abdominal aorta terminates when it bifurcates into the two common iliac arteries at the level of the fourth lumbar vertebra. See Figure 3 for an illustration of the ascending aorta, the aortic arch, and the initial segment of the descending aorta plus major branches; Table 3 summarizes the structures of the aorta.

Figure 3. The aorta has distinct regions, including the ascending aorta, aortic arch, and the descending aorta, which includes the thoracic and abdominal regions.
Coronary Circulation
The first vessels that branch from the ascending aorta are the paired coronary arteries, which arise from two of the three sinuses in the ascending aorta just superior to the aortic semilunar valve. These sinuses contain the aortic baroreceptors and chemoreceptors critical to maintain cardiac function. The left coronary artery arises from the left posterior aortic sinus. The right coronary artery arises from the anterior aortic sinus. Normally, the right posterior aortic sinus does not give rise to a vessel.
The coronary arteries encircle the heart, forming a ring-like structure that divides into the next level of branches that supplies blood to the heart tissues. (Seek additional content for more detail on cardiac circulation.)
Aortic Arch Branches
There are three major branches of the aortic arch: the brachiocephalic artery, the left common carotid artery, and the left subclavian (literally “under the clavicle”) artery. As you would expect based upon proximity to the heart, each of these vessels is classified as an elastic artery.
The brachiocephalic artery is located only on the right side of the body; there is no corresponding artery on the left. The brachiocephalic artery branches into the right subclavian artery and the right common carotid artery. The left subclavian and left common carotid arteries arise independently from the aortic arch but otherwise follow a similar pattern and distribution to the corresponding arteries on the right side (see Figure 2).
Each subclavian artery supplies blood to the arms, chest, shoulders, back, and central nervous system. It then gives rise to three major branches: the internal thoracic artery, the vertebral artery, and the thyrocervical artery. The internal thoracic artery , or mammary artery, supplies blood to the thymus, the pericardium of the heart, and the anterior chest wall. The vertebral artery passes through the vertebral foramen in the cervical vertebrae and then through the foramen magnum into the cranial cavity to supply blood to the brain and spinal cord. The paired vertebral arteries join together to form the large basilar artery at the base of the medulla oblongata. This is an example of an anastomosis. The subclavian artery also gives rise to the thyrocervical artery that provides blood to the thyroid, the cervical region of the neck, and the upper back and shoulder.
The common carotid artery divides into internal and external carotid arteries. The right common carotid artery arises from the brachiocephalic artery and the left common carotid artery arises directly from the aortic arch. The external carotid artery supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx. These branches include the lingual, facial, occipital, maxillary, and superficial temporal arteries. The internal carotid artery initially forms an expansion known as the carotid sinus, containing the carotid baroreceptors and chemoreceptors. Like their counterparts in the aortic sinuses, the information provided by these receptors is critical to maintaining cardiovascular homeostasis (see Figure 2).
The internal carotid arteries along with the vertebral arteries are the two primary suppliers of blood to the human brain. Given the central role and vital importance of the brain to life, it is critical that blood supply to this organ remains uninterrupted. Recall that blood flow to the brain is remarkably constant, with approximately 20 percent of blood flow directed to this organ at any given time. When blood flow is interrupted, even for just a few seconds, a transient ischemic attack (TIA) , or mini-stroke, may occur, resulting in loss of consciousness or temporary loss of neurological function. In some cases, the damage may be permanent. Loss of blood flow for longer periods, typically between 3 and 4 minutes, will likely produce irreversible brain damage or a stroke, also called a cerebrovascular accident (CVA) . The locations of the arteries in the brain not only provide blood flow to the brain tissue but also prevent interruption in the flow of blood. Both the carotid and vertebral arteries branch once they enter the cranial cavity, and some of these branches form a structure known as the arterial circle (or circle of Willis ), an anastomosis that is remarkably like a traffic circle that sends off branches (in this case, arterial branches to the brain). As a rule, branches to the anterior portion of the cerebrum are normally fed by the internal carotid arteries; the remainder of the brain receives blood flow from branches associated with the vertebral arteries.

Figure 4. The common carotid artery gives rise to the external and internal carotid arteries. The external carotid artery remains superficial and gives rise to many arteries of the head. The internal carotid artery first forms the carotid sinus and then reaches the brain via the carotid canal and carotid foramen, emerging into the cranium via the foramen lacerum. The vertebral artery branches from the subclavian artery and passes through the transverse foramen in the cervical vertebrae, entering the base of the skull at the vertebral foramen. The subclavian artery continues toward the arm as the axillary artery.
The internal carotid artery continues through the carotid canal of the temporal bone and enters the base of the brain through the carotid foramen where it gives rise to several branches (see Figure 4 and Figure 5).
One of these branches is the anterior cerebral artery that supplies blood to the frontal lobe of the cerebrum. Another branch, the middle cerebral artery , supplies blood to the temporal and parietal lobes, which are the most common sites of CVAs. The ophthalmic artery , the third major branch, provides blood to the eyes.
The right and left anterior cerebral arteries join together to form an anastomosis called the anterior communicating artery . The initial segments of the anterior cerebral arteries and the anterior communicating artery form the anterior portion of the arterial circle. The posterior portion of the arterial circle is formed by a left and a right posterior communicating artery that branches from the posterior cerebral artery , which arises from the basilar artery. It provides blood to the posterior portion of the cerebrum and brain stem. The basilar artery is an anastomosis that begins at the junction of the two vertebral arteries and sends branches to the cerebellum and brain stem. It flows into the posterior cerebral arteries. Table 4 summarizes the aortic arch branches, including the major branches supplying the brain.

Figure 5. This inferior view shows the network of arteries serving the brain. The structure is referred to as the arterial circle or circle of Willis.
Thoracic Aorta and Major Branches
The thoracic aorta begins at the level of vertebra T5 and continues through to the diaphragm at the level of T12, initially traveling within the mediastinum to the left of the vertebral column. As it passes through the thoracic region, the thoracic aorta gives rise to several branches, which are collectively referred to as visceral branches and parietal branches. Those branches that supply blood primarily to visceral organs are known as the visceral branches and include the bronchial arteries, pericardial arteries, esophageal arteries, and the mediastinal arteries, each named after the tissues it supplies. Each bronchial artery (typically two on the left and one on the right) supplies systemic blood to the lungs and visceral pleura, in addition to the blood pumped to the lungs for oxygenation via the pulmonary circuit. The bronchial arteries follow the same path as the respiratory branches, beginning with the bronchi and ending with the bronchioles. There is considerable, but not total, intermingling of the systemic and pulmonary blood at anastomoses in the smaller branches of the lungs. This may sound incongruous—that is, the mixing of systemic arterial blood high in oxygen with the pulmonary arterial blood lower in oxygen—but the systemic vessels also deliver nutrients to the lung tissue just as they do elsewhere in the body. The mixed blood drains into typical pulmonary veins, whereas the bronchial artery branches remain separate and drain into bronchial veins described later. Each pericardial artery supplies blood to the pericardium, the esophageal artery provides blood to the esophagus, and the mediastinal artery provides blood to the mediastinum. The remaining thoracic aorta branches are collectively referred to as parietal branches or somatic branches, and include the intercostal and superior phrenic arteries. Each intercostal artery provides blood to the muscles of the thoracic cavity and vertebral column. The superior phrenic artery provides blood to the superior surface of the diaphragm. The image and table below lists the arteries of the thoracic region.

Figure 6. The thoracic aorta gives rise to the arteries of the visceral and parietal branches.
Abdominal Aorta and Major Branches
After crossing through the diaphragm at the aortic hiatus, the thoracic aorta is called the abdominal aorta (Figure 6). This vessel remains to the left of the vertebral column and is embedded in adipose tissue behind the peritoneal cavity. It formally ends at approximately the level of vertebra L4, where it bifurcates to form the common iliac arteries. Before this division, the abdominal aorta gives rise to several important branches. A single celiac trunk (artery) emerges and divides into the left gastric artery to supply blood to the stomach and esophagus, the splenic artery to supply blood to the spleen, and the common hepatic artery , which in turn gives rise to the hepatic artery proper to supply blood to the liver, the right gastric artery to supply blood to the stomach, the cystic artery to supply blood to the gall bladder, and several branches, one to supply blood to the duodenum and another to supply blood to the pancreas. Two additional single vessels arise from the abdominal aorta. These are the superior and inferior mesenteric arteries. The superior mesenteric artery arises approximately 2.5 cm after the celiac trunk and branches into several major vessels that supply blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine. The inferior mesenteric artery supplies blood to the distal segment of the large intestine, including the rectum. It arises approximately 5 cm superior to the common iliac arteries.
In addition to these single branches, the abdominal aorta gives rise to several significant paired arteries along the way. These include the inferior phrenic arteries, the adrenal arteries, the renal arteries, the gonadal arteries, and the lumbar arteries. Each inferior phrenic artery is a counterpart of a superior phrenic artery and supplies blood to the inferior surface of the diaphragm. The adrenal artery supplies blood to the adrenal (suprarenal) glands and arises near the superior mesenteric artery. Each renal artery branches approximately 2.5 cm inferior to the superior mesenteric arteries and supplies a kidney. The right renal artery is longer than the left since the aorta lies to the left of the vertebral column and the vessel must travel a greater distance to reach its target. Renal arteries branch repeatedly to supply blood to the kidneys. Each gonadal artery supplies blood to the gonads, or reproductive organs, and is also described as either an ovarian artery or a testicular artery (internal spermatic), depending upon the sex of the individual. An ovarian artery supplies blood to an ovary, uterine (Fallopian) tube, and the uterus, and is located within the suspensory ligament of the uterus. It is considerably shorter than a testicular artery , which ultimately travels outside the body cavity to the testes, forming one component of the spermatic cord. The gonadal arteries arise inferior to the renal arteries and are generally retroperitoneal. The ovarian artery continues to the uterus where it forms an anastomosis with the uterine artery that supplies blood to the uterus. Both the uterine arteries and vaginal arteries, which distribute blood to the vagina, are branches of the internal iliac artery. The four paired lumbar arteries are the counterparts of the intercostal arteries and supply blood to the lumbar region, the abdominal wall, and the spinal cord. In some instances, a fifth pair of lumbar arteries emerges from the median sacral artery.
The aorta divides at approximately the level of vertebra L4 into a left and a right common iliac artery but continues as a small vessel, the median sacral artery , into the sacrum. The common iliac arteries provide blood to the pelvic region and ultimately to the lower limbs. They split into external and internal iliac arteries approximately at the level of the lumbar-sacral articulation. Each internal iliac artery sends branches to the urinary bladder, the walls of the pelvis, the external genitalia, and the medial portion of the femoral region. In females, they also provide blood to the uterus and vagina. The much larger external iliac artery supplies blood to each of the lower limbs. Figure 8 shows the distribution of the major branches of the aorta into the thoracic and abdominal regions. Figure 9 shows the distribution of the major branches of the common iliac arteries.

Figure 7. The flow chart summarizes the distribution of the major branches of the aorta into the thoracic and abdominal regions.

Figure 8. The flow chart below summarizes the distribution of the major branches of the common iliac arteries into the pelvis and lower limbs. The left side follows a similar pattern to the right.
Table 6 summarizes the major branches of the abdominal aorta.
Arteries Serving the Upper Limbs

Figure 9. The arteries that supply blood to the arms and hands are extensions of the subclavian arteries.
As the subclavian artery exits the thorax into the axillary region, it is renamed the axillary artery . Although it does branch and supply blood to the region near the head of the humerus (via the humeral circumflex arteries), the majority of the vessel continues into the upper arm, or brachium, and becomes the brachial artery (Figure 9).
The brachial artery supplies blood to much of the brachial region and divides at the elbow into several smaller branches, including the deep brachial arteries, which provide blood to the posterior surface of the arm, and the ulnar collateral arteries, which supply blood to the region of the elbow.
As the brachial artery approaches the coronoid fossa, it bifurcates into the radial and ulnar arteries, which continue into the forearm, or antebrachium. The radial artery and ulnar artery parallel their namesake bones, giving off smaller branches until they reach the wrist, or carpal region. At this level, they fuse to form the superficial and deep palmar arches that supply blood to the hand, as well as the digital arteries that supply blood to the digits. Figure 9 show the distribution of systemic arteries from the heart into the upper limb. Table 7 summarizes the arteries serving the upper limbs.

Figure 10. The flow chart summarizes the distribution of the major arteries from the heart into the upper limb.
Arteries Serving the Lower Limbs
The external iliac artery exits the body cavity and enters the femoral region of the lower leg (Figure 11). As it passes through the body wall, it is renamed the femoral artery . It gives off several smaller branches as well as the lateral deep femoral artery that in turn gives rise to a lateral circumflex artery . These arteries supply blood to the deep muscles of the thigh as well as ventral and lateral regions of the integument. The femoral artery also gives rise to the genicular artery , which provides blood to the region of the knee. As the femoral artery passes posterior to the knee near the popliteal fossa, it is called the popliteal artery. The popliteal artery branches into the anterior and posterior tibial arteries.

Figure 11. Major arteries serving the lower limb are shown in anterior and posterior views.
The anterior tibial artery is located between the tibia and fibula, and supplies blood to the muscles and integument of the anterior tibial region. Upon reaching the tarsal region, it becomes the dorsalis pedis artery , which branches repeatedly and provides blood to the tarsal and dorsal regions of the foot. The posterior tibial artery provides blood to the muscles and integument on the posterior surface of the tibial region. The fibular or peroneal artery branches from the posterior tibial artery. It bifurcates and becomes the medial plantar artery and lateral plantar artery , providing blood to the plantar surfaces. There is an anastomosis with the dorsalis pedis artery, and the medial and lateral plantar arteries form two arches called the dorsal arch (also called the arcuate arch) and the plantar arch , which provide blood to the remainder of the foot and toes. Figure 12 show the distribution of the major systemic arteries in the lower limb. Table 8 summarizes the major systemic arteries discussed in the text.

Figure 12. The flow chart summarizes the distribution of the systemic arteries from the external iliac artery into the lower limb.
Overview of Systemic Veins
Systemic veins return blood to the right atrium. Since the blood has already passed through the systemic capillaries, it will be relatively low in oxygen concentration. In many cases, there will be veins draining organs and regions of the body with the same name as the arteries that supplied these regions and the two often parallel one another. This is often described as a “complementary” pattern. However, there is a great deal more variability in the venous circulation than normally occurs in the arteries. For the sake of brevity and clarity, this text will discuss only the most commonly encountered patterns. However, keep this variation in mind when you move from the classroom to clinical practice.
In both the neck and limb regions, there are often both superficial and deeper levels of veins. The deeper veins generally correspond to the complementary arteries. The superficial veins do not normally have direct arterial counterparts, but in addition to returning blood, they also make contributions to the maintenance of body temperature. When the ambient temperature is warm, more blood is diverted to the superficial veins where heat can be more easily dissipated to the environment. In colder weather, there is more constriction of the superficial veins and blood is diverted deeper where the body can retain more of the heat.
The “Voyage of Discovery” analogy and stick drawings mentioned earlier remain valid techniques for the study of systemic veins, but veins present a more difficult challenge because there are numerous anastomoses and multiple branches. It is like following a river with many tributaries and channels, several of which interconnect. Tracing blood flow through arteries follows the current in the direction of blood flow, so that we move from the heart through the large arteries and into the smaller arteries to the capillaries. From the capillaries, we move into the smallest veins and follow the direction of blood flow into larger veins and back to the heart. Figure 13 outlines the path of the major systemic veins.

Figure 13. The major systemic veins of the body are shown here in an anterior view.
The right atrium receives all of the systemic venous return. Most of the blood flows into either the superior vena cava or inferior vena cava. If you draw an imaginary line at the level of the diaphragm, systemic venous circulation from above that line will generally flow into the superior vena cava; this includes blood from the head, neck, chest, shoulders, and upper limbs. The exception to this is that most venous blood flow from the coronary veins flows directly into the coronary sinus and from there directly into the right atrium. Beneath the diaphragm, systemic venous flow enters the inferior vena cava, that is, blood from the abdominal and pelvic regions and the lower limbs.
The Superior Vena Cava
The superior vena cava drains most of the body superior to the diaphragm. On both the left and right sides, the subclavian vein forms when the axillary vein passes through the body wall from the axillary region. It fuses with the external and internal jugular veins from the head and neck to form the brachiocephalic vein . Each vertebral vein also flows into the brachiocephalic vein close to this fusion. These veins arise from the base of the brain and the cervical region of the spinal cord, and flow largely through the intervertebral foramina in the cervical vertebrae. They are the counterparts of the vertebral arteries. Each internal thoracic vein , also known as an internal mammary vein, drains the anterior surface of the chest wall and flows into the brachiocephalic vein.
The remainder of the blood supply from the thorax drains into the azygos vein. Each intercostal vein drains muscles of the thoracic wall, each esophageal vein delivers blood from the inferior portions of the esophagus, each bronchial vein drains the systemic circulation from the lungs, and several smaller veins drain the mediastinal region. Bronchial veins carry approximately 13 percent of the blood that flows into the bronchial arteries; the remainder intermingles with the pulmonary circulation and returns to the heart via the pulmonary veins. These veins flow into the azygos vein , and with the smaller hemiazygos vein ( hemi – = “half”) on the left of the vertebral column, drain blood from the thoracic region. The hemiazygos vein does not drain directly into the superior vena cava but enters the brachiocephalic vein via the superior intercostal vein.
The azygos vein passes through the diaphragm from the thoracic cavity on the right side of the vertebral column and begins in the lumbar region of the thoracic cavity. It flows into the superior vena cava at approximately the level of T2, making a significant contribution to the flow of blood. It combines with the two large left and right brachiocephalic veins to form the superior vena cava.
Figure 14 and Table 9 summarize the veins of the thoracic region that flow into the superior vena cava.

Figure 14. Veins of the thoracic and abdominal regions drain blood from the area above the diaphragm, returning it to the right atrium via the superior vena cava.
Veins of the Head and Neck
Blood from the brain and the superficial facial vein flow into each internal jugular vein . Blood from the more superficial portions of the head, scalp, and cranial regions, including the temporal vein and maxillary vein , flow into each external jugular vein . Although the external and internal jugular veins are separate vessels, there are anastomoses between them close to the thoracic region. Blood from the external jugular vein empties into the subclavian vein. Table 10 summarizes the major veins of the head and neck.
Venous Drainage of the Brain
Circulation to the brain is both critical and complex. Many smaller veins of the brain stem and the superficial veins of the cerebrum lead to larger vessels referred to as intracranial sinuses. These include the superior and inferior sagittal sinuses, straight sinus, cavernous sinuses, left and right sinuses, the petrosal sinuses, and the occipital sinuses. Ultimately, sinuses will lead back to either the inferior jugular vein or vertebral vein.
Most of the veins on the superior surface of the cerebrum flow into the largest of the sinuses, the superior sagittal sinus . It is located midsagittally between the meningeal and periosteal layers of the dura mater within the falx cerebri and, at first glance in images or models, can be mistaken for the subarachnoid space. Most reabsorption of cerebrospinal fluid occurs via the chorionic villi (arachnoid granulations) into the superior sagittal sinus. Blood from most of the smaller vessels originating from the inferior cerebral veins flows into the great cerebral vein and into the straight sinus . Other cerebral veins and those from the eye socket flow into the cavernous sinus , which flows into the petrosal sinus and then into the internal jugular vein. The occipital sinus , sagittal sinus, and straight sinuses all flow into the left and right transverse sinuses near the lambdoid suture. The transverse sinuses in turn flow into the sigmoid sinuses that pass through the jugular foramen and into the internal jugular vein. The internal jugular vein flows parallel to the common carotid artery and is more or less its counterpart. It empties into the brachiocephalic vein. The veins draining the cervical vertebrae and the posterior surface of the skull, including some blood from the occipital sinus, flow into the vertebral veins. These parallel the vertebral arteries and travel through the transverse foramina of the cervical vertebrae. The vertebral veins also flow into the brachiocephalic veins. Figure 15 and Table 11 summarize the major veins of the brain.

Figure 15. This left lateral view shows the veins of the head and neck, including the intercranial sinuses.
Veins Draining the Upper Limbs

Figure 16. This anterior view shows the veins that drain the upper limb.
The digital veins in the fingers come together in the hand to form the palmar venous arches (Figure 16). From here, the veins come together to form the radial vein, the ulnar vein, and the median antebrachial vein. The radial vein and the ulnar vein parallel the bones of the forearm and join together at the antebrachium to form the brachial vein , a deep vein that flows into the axillary vein in the brachium.
The median antebrachial vein parallels the ulnar vein, is more medial in location, and joins the basilic vein in the forearm. As the basilic vein reaches the antecubital region, it gives off a branch called the median cubital vein that crosses at an angle to join the cephalic vein. The median cubital vein is the most common site for drawing venous blood in humans. The basilic vein continues through the arm medially and superficially to the axillary vein.
The cephalic vein begins in the antebrachium and drains blood from the superficial surface of the arm into the axillary vein. It is extremely superficial and easily seen along the surface of the biceps brachii muscle in individuals with good muscle tone and in those without excessive subcutaneous adipose tissue in the arms.
The subscapular vein drains blood from the subscapular region and joins the cephalic vein to form the axillary vein . As it passes through the body wall and enters the thorax, the axillary vein becomes the subclavian vein.
Many of the larger veins of the thoracic and abdominal region and upper limb are further represented in the flow chart below. Figure 17 and Table 12 summarize the veins of the upper limbs.

Figure 17. The flow chart summarizes the distribution of the veins flowing into the superior vena cava.
The Inferior Vena Cava
Other than the small amount of blood drained by the azygos and hemiazygos veins, most of the blood inferior to the diaphragm drains into the inferior vena cava before it is returned to the heart (see Figure 15). Lying just beneath the parietal peritoneum in the abdominal cavity, the inferior vena cava parallels the abdominal aorta, where it can receive blood from abdominal veins. The lumbar portions of the abdominal wall and spinal cord are drained by a series of lumbar veins , usually four on each side. The ascending lumbar veins drain into either the azygos vein on the right or the hemiazygos vein on the left, and return to the superior vena cava. The remaining lumbar veins drain directly into the inferior vena cava.
Blood supply from the kidneys flows into each renal vein , normally the largest veins entering the inferior vena cava. A number of other, smaller veins empty into the left renal vein. Each adrenal vein drains the adrenal or suprarenal glands located immediately superior to the kidneys. The right adrenal vein enters the inferior vena cava directly, whereas the left adrenal vein enters the left renal vein.
From the male reproductive organs, each testicular vein flows from the scrotum, forming a portion of the spermatic cord. Each ovarian vein drains an ovary in females. Each of these veins is generically called a gonadal vein . The right gonadal vein empties directly into the inferior vena cava, and the left gonadal vein empties into the left renal vein.
Each side of the diaphragm drains into a phrenic vein ; the right phrenic vein empties directly into the inferior vena cava, whereas the left phrenic vein empties into the left renal vein. Blood supply from the liver drains into each hepatic vein and directly into the inferior vena cava. Since the inferior vena cava lies primarily to the right of the vertebral column and aorta, the left renal vein is longer, as are the left phrenic, adrenal, and gonadal veins. The longer length of the left renal vein makes the left kidney the primary target of surgeons removing this organ for donation. Figure 18 provides a flow chart of the veins flowing into the inferior vena cava. Table 13 summarizes the major veins of the abdominal region.

Figure 18. The flow chart summarizes veins that deliver blood to the inferior vena cava.
Veins Draining the Lower Limbs
The superior surface of the foot drains into the digital veins, and the inferior surface drains into the plantar veins , which flow into a complex series of anastomoses in the feet and ankles, including the dorsal venous arch and the plantar venous arch . From the dorsal venous arch, blood supply drains into the anterior and posterior tibial veins. The anterior tibial vein drains the area near the tibialis anterior muscle and combines with the posterior tibial vein and the fibular vein to form the popliteal vein. The posterior tibial vein drains the posterior surface of the tibia and joins the popliteal vein. The fibular vein drains the muscles and integument in proximity to the fibula and also joins the popliteal vein. The small saphenous vein located on the lateral surface of the leg drains blood from the superficial regions of the lower leg and foot, and flows into to the popliteal vein . As the popliteal vein passes behind the knee in the popliteal region, it becomes the femoral vein. It is palpable in patients without excessive adipose tissue.

Figure 19. Anterior and posterior views show the major veins that drain the lower limb into the inferior vena cava.
Close to the body wall, the great saphenous vein, the deep femoral vein, and the femoral circumflex vein drain into the femoral vein. The great saphenous vein is a prominent surface vessel located on the medial surface of the leg and thigh that collects blood from the superficial portions of these areas. The deep femoral vein , as the name suggests, drains blood from the deeper portions of the thigh. The femoral circumflex vein forms a loop around the femur just inferior to the trochanters and drains blood from the areas in proximity to the head and neck of the femur.
As the femoral vein penetrates the body wall from the femoral portion of the upper limb, it becomes the external iliac vein , a large vein that drains blood from the leg to the common iliac vein. The pelvic organs and integument drain into the internal iliac vein , which forms from several smaller veins in the region, including the umbilical veins that run on either side of the bladder. The external and internal iliac veins combine near the inferior portion of the sacroiliac joint to form the common iliac vein. In addition to blood supply from the external and internal iliac veins, the middle sacral vein drains the sacral region into the common iliac vein . Similar to the common iliac arteries, the common iliac veins come together at the level of L5 to form the inferior vena cava.
Figure 20 is a flow chart of veins flowing into the lower limb. Table 14 summarizes the major veins of the lower limbs.

Figure 20. The flow chart summarizes venous flow from the lower limb.
Hepatic Portal System

Figure 22. The liver receives blood from the normal systemic circulation via the hepatic artery. It also receives and processes blood from other organs, delivered via the veins of the hepatic portal system. All blood exits the liver via the hepatic vein, which delivers the blood to the inferior vena cava. (Different colors are used to help distinguish among the different vessels in the system.)
The liver is a complex biochemical processing plant. It packages nutrients absorbed by the digestive system; produces plasma proteins, clotting factors, and bile; and disposes of worn-out cell components and waste products. Instead of entering the circulation directly, absorbed nutrients and certain wastes (for example, materials produced by the spleen) travel to the liver for processing. They do so via the hepatic portal system . Portal systems begin and end in capillaries. In this case, the initial capillaries from the stomach, small intestine, large intestine, and spleen lead to the hepatic portal vein and end in specialized capillaries within the liver, the hepatic sinusoids. You saw the only other portal system with the hypothalamic-hypophyseal portal vessel in the endocrine chapter.
The hepatic portal system consists of the hepatic portal vein and the veins that drain into it. The hepatic portal vein itself is relatively short, beginning at the level of L2 with the confluence of the superior mesenteric and splenic veins. It also receives branches from the inferior mesenteric vein, plus the splenic veins and all their tributaries. The superior mesenteric vein receives blood from the small intestine, two-thirds of the large intestine, and the stomach. The inferior mesenteric vein drains the distal third of the large intestine, including the descending colon, the sigmoid colon, and the rectum. The splenic vein is formed from branches from the spleen, pancreas, and portions of the stomach, and the inferior mesenteric vein. After its formation, the hepatic portal vein also receives branches from the gastric veins of the stomach and cystic veins from the gall bladder. The hepatic portal vein delivers materials from these digestive and circulatory organs directly to the liver for processing.
Because of the hepatic portal system, the liver receives its blood supply from two different sources: from normal systemic circulation via the hepatic artery and from the hepatic portal vein. The liver processes the blood from the portal system to remove certain wastes and excess nutrients, which are stored for later use. This processed blood, as well as the systemic blood that came from the hepatic artery, exits the liver via the right, left, and middle hepatic veins, and flows into the inferior vena cava. Overall systemic blood composition remains relatively stable, since the liver is able to metabolize the absorbed digestive components.
Chapter Review
The right ventricle pumps oxygen-depleted blood into the pulmonary trunk and right and left pulmonary arteries, which carry it to the right and left lungs for gas exchange. Oxygen-rich blood is transported by pulmonary veins to the left atrium. The left ventricle pumps this blood into the aorta. The main regions of the aorta are the ascending aorta, aortic arch, and descending aorta, which is further divided into the thoracic and abdominal aorta. The coronary arteries branch from the ascending aorta. After oxygenating tissues in the capillaries, systemic blood is returned to the right atrium from the venous system via the superior vena cava, which drains most of the veins superior to the diaphragm, the inferior vena cava, which drains most of the veins inferior to the diaphragm, and the coronary veins via the coronary sinus. The hepatic portal system carries blood to the liver for processing before it enters circulation. Review the figures provided in this section for circulation of blood through the blood vessels.
Critical Thinking Questions
- Identify the ventricle of the heart that pumps oxygen-depleted blood and the arteries of the body that carry oxygen-depleted blood.
- What organs do the gonadal veins drain?
- What arteries play the leading roles in supplying blood to the brain?
- The right ventricle of the heart pumps oxygen-depleted blood to the pulmonary arteries.
- The gonadal veins drain the testes in males and the ovaries in females.
- The internal carotid arteries and the vertebral arteries provide most of the brain’s blood supply.
abdominal aorta: portion of the aorta inferior to the aortic hiatus and superior to the common iliac arteries
adrenal artery: branch of the abdominal aorta; supplies blood to the adrenal (suprarenal) glands
adrenal vein: drains the adrenal or suprarenal glands that are immediately superior to the kidneys; the right adrenal vein enters the inferior vena cava directly and the left adrenal vein enters the left renal vein
anterior cerebral artery: arises from the internal carotid artery; supplies the frontal lobe of the cerebrum
anterior communicating artery: anastomosis of the right and left internal carotid arteries; supplies blood to the brain
anterior tibial artery: branches from the popliteal artery; supplies blood to the anterior tibial region; becomes the dorsalis pedis artery
anterior tibial vein: forms from the dorsal venous arch; drains the area near the tibialis anterior muscle and leads to the popliteal vein
aorta: largest artery in the body, originating from the left ventricle and descending to the abdominal region where it bifurcates into the common iliac arteries at the level of the fourth lumbar vertebra; arteries originating from the aorta distribute blood to virtually all tissues of the body
aortic arch: arc that connects the ascending aorta to the descending aorta; ends at the intervertebral disk between the fourth and fifth thoracic vertebrae
aortic hiatus: opening in the diaphragm that allows passage of the thoracic aorta into the abdominal region where it becomes the abdominal aorta
arterial circle: (also, circle of Willis) anastomosis located at the base of the brain that ensures continual blood supply; formed from branches of the internal carotid and vertebral arteries; supplies blood to the brain
ascending aorta: initial portion of the aorta, rising from the left ventricle for a distance of approximately 5 cm
axillary artery: continuation of the subclavian artery as it penetrates the body wall and enters the axillary region; supplies blood to the region near the head of the humerus (humeral circumflex arteries); the majority of the vessel continues into the brachium and becomes the brachial artery
axillary vein: major vein in the axillary region; drains the upper limb and becomes the subclavian vein
azygos vein: originates in the lumbar region and passes through the diaphragm into the thoracic cavity on the right side of the vertebral column; drains blood from the intercostal veins, esophageal veins, bronchial veins, and other veins draining the mediastinal region; leads to the superior vena cava
basilar artery: formed from the fusion of the two vertebral arteries; sends branches to the cerebellum, brain stem, and the posterior cerebral arteries; the main blood supply to the brain stem
basilic vein: superficial vein of the arm that arises from the palmar venous arches, intersects with the median cubital vein, parallels the ulnar vein, and continues into the upper arm; along with the brachial vein, it leads to the axillary vein
brachial artery: continuation of the axillary artery in the brachium; supplies blood to much of the brachial region; gives off several smaller branches that provide blood to the posterior surface of the arm in the region of the elbow; bifurcates into the radial and ulnar arteries at the coronoid fossa
brachial vein: deeper vein of the arm that forms from the radial and ulnar veins in the lower arm; leads to the axillary vein
brachiocephalic artery: single vessel located on the right side of the body; the first vessel branching from the aortic arch; gives rise to the right subclavian artery and the right common carotid artery; supplies blood to the head, neck, upper limb, and wall of the thoracic region
brachiocephalic vein: one of a pair of veins that form from a fusion of the external and internal jugular veins and the subclavian vein; subclavian, external and internal jugulars, vertebral, and internal thoracic veins lead to it; drains the upper thoracic region and flows into the superior vena cava
bronchial artery: systemic branch from the aorta that provides oxygenated blood to the lungs in addition to the pulmonary circuit
bronchial vein: drains the systemic circulation from the lungs and leads to the azygos vein
cavernous sinus: enlarged vein that receives blood from most of the other cerebral veins and the eye socket, and leads to the petrosal sinus
celiac trunk: (also, celiac artery) major branch of the abdominal aorta; gives rise to the left gastric artery, the splenic artery, and the common hepatic artery that forms the hepatic artery to the liver, the right gastric artery to the stomach, and the cystic artery to the gall bladder
cephalic vein: superficial vessel in the upper arm; leads to the axillary vein
cerebrovascular accident (CVA): blockage of blood flow to the brain; also called a stroke
circle of Willis: (also, arterial circle) anastomosis located at the base of the brain that ensures continual blood supply; formed from branches of the internal carotid and vertebral arteries; supplies blood to the brain
common carotid artery: right common carotid artery arises from the brachiocephalic artery, and the left common carotid arises from the aortic arch; gives rise to the external and internal carotid arteries; supplies the respective sides of the head and neck
common hepatic artery: branch of the celiac trunk that forms the hepatic artery, the right gastric artery, and the cystic artery
common iliac artery: branch of the aorta that leads to the internal and external iliac arteries
common iliac vein: one of a pair of veins that flows into the inferior vena cava at the level of L5; the left common iliac vein drains the sacral region; divides into external and internal iliac veins near the inferior portion of the sacroiliac joint
cystic artery: branch of the common hepatic artery; supplies blood to the gall bladder
deep femoral artery: branch of the femoral artery; gives rise to the lateral circumflex arteries
deep femoral vein: drains blood from the deeper portions of the thigh and leads to the femoral vein
descending aorta: portion of the aorta that continues downward past the end of the aortic arch; subdivided into the thoracic aorta and the abdominal aorta
digital arteries: formed from the superficial and deep palmar arches; supply blood to the digits
digital veins: drain the digits and feed into the palmar arches of the hand and dorsal venous arch of the foot
dorsal arch: (also, arcuate arch) formed from the anastomosis of the dorsalis pedis artery and medial and plantar arteries; branches supply the distal portions of the foot and digits
dorsal venous arch: drains blood from digital veins and vessels on the superior surface of the foot
dorsalis pedis artery: forms from the anterior tibial artery; branches repeatedly to supply blood to the tarsal and dorsal regions of the foot
esophageal artery: branch of the thoracic aorta; supplies blood to the esophagus
esophageal vein: drains the inferior portions of the esophagus and leads to the azygos vein
external carotid artery: arises from the common carotid artery; supplies blood to numerous structures within the face, lower jaw, neck, esophagus, and larynx
external iliac artery: branch of the common iliac artery that leaves the body cavity and becomes a femoral artery; supplies blood to the lower limbs
external iliac vein: formed when the femoral vein passes into the body cavity; drains the legs and leads to the common iliac vein
external jugular vein: one of a pair of major veins located in the superficial neck region that drains blood from the more superficial portions of the head, scalp, and cranial regions, and leads to the subclavian vein
femoral artery: continuation of the external iliac artery after it passes through the body cavity; divides into several smaller branches, the lateral deep femoral artery, and the genicular artery; becomes the popliteal artery as it passes posterior to the knee
femoral circumflex vein: forms a loop around the femur just inferior to the trochanters; drains blood from the areas around the head and neck of the femur; leads to the femoral vein
femoral vein: drains the upper leg; receives blood from the great saphenous vein, the deep femoral vein, and the femoral circumflex vein; becomes the external iliac vein when it crosses the body wall
fibular vein: drains the muscles and integument near the fibula and leads to the popliteal vein
genicular artery: branch of the femoral artery; supplies blood to the region of the knee
gonadal artery: branch of the abdominal aorta; supplies blood to the gonads or reproductive organs; also described as ovarian arteries or testicular arteries, depending upon the sex of the individual
gonadal vein: generic term for a vein draining a reproductive organ; may be either an ovarian vein or a testicular vein, depending on the sex of the individual
great cerebral vein: receives most of the smaller vessels from the inferior cerebral veins and leads to the straight sinus
great saphenous vein: prominent surface vessel located on the medial surface of the leg and thigh; drains the superficial portions of these areas and leads to the femoral vein
hemiazygos vein: smaller vein complementary to the azygos vein; drains the esophageal veins from the esophagus and the left intercostal veins, and leads to the brachiocephalic vein via the superior intercostal vein
hepatic artery proper: branch of the common hepatic artery; supplies systemic blood to the liver
hepatic portal system: specialized circulatory pathway that carries blood from digestive organs to the liver for processing before being sent to the systemic circulation
hepatic vein: drains systemic blood from the liver and flows into the inferior vena cava
inferior mesenteric artery: branch of the abdominal aorta; supplies blood to the distal segment of the large intestine and rectum
inferior phrenic artery: branch of the abdominal aorta; supplies blood to the inferior surface of the diaphragm
inferior vena cava: large systemic vein that drains blood from areas largely inferior to the diaphragm; empties into the right atrium
intercostal artery: branch of the thoracic aorta; supplies blood to the muscles of the thoracic cavity and vertebral column
intercostal vein: drains the muscles of the thoracic wall and leads to the azygos vein
internal carotid artery: arises from the common carotid artery and begins with the carotid sinus; goes through the carotid canal of the temporal bone to the base of the brain; combines with branches of the vertebral artery forming the arterial circle; supplies blood to the brain
internal iliac artery: branch from the common iliac arteries; supplies blood to the urinary bladder, walls of the pelvis, external genitalia, and the medial portion of the femoral region; in females, also provide blood to the uterus and vagina
internal iliac vein: drains the pelvic organs and integument; formed from several smaller veins in the region; leads to the common iliac vein
internal jugular vein: one of a pair of major veins located in the neck region that passes through the jugular foramen and canal, flows parallel to the common carotid artery that is more or less its counterpart; primarily drains blood from the brain, receives the superficial facial vein, and empties into the subclavian vein
internal thoracic artery: (also, mammary artery) arises from the subclavian artery; supplies blood to the thymus, pericardium of the heart, and the anterior chest wall
internal thoracic vein: (also, internal mammary vein) drains the anterior surface of the chest wall and leads to the brachiocephalic vein
lateral circumflex artery: branch of the deep femoral artery; supplies blood to the deep muscles of the thigh and the ventral and lateral regions of the integument
lateral plantar artery: arises from the bifurcation of the posterior tibial arteries; supplies blood to the lateral plantar surfaces of the foot
left gastric artery: branch of the celiac trunk; supplies blood to the stomach
lumbar arteries: branches of the abdominal aorta; supply blood to the lumbar region, the abdominal wall, and spinal cord
lumbar veins: drain the lumbar portion of the abdominal wall and spinal cord; the superior lumbar veins drain into the azygos vein on the right or the hemiazygos vein on the left; blood from these vessels is returned to the superior vena cava rather than the inferior vena cava
maxillary vein: drains blood from the maxillary region and leads to the external jugular vein
medial plantar artery: arises from the bifurcation of the posterior tibial arteries; supplies blood to the medial plantar surfaces of the foot
median antebrachial vein: vein that parallels the ulnar vein but is more medial in location; intertwines with the palmar venous arches
median cubital vein: superficial vessel located in the antecubital region that links the cephalic vein to the basilic vein in the form of a v; a frequent site for a blood draw
median sacral artery: continuation of the aorta into the sacrum
mediastinal artery: branch of the thoracic aorta; supplies blood to the mediastinum
middle cerebral artery: another branch of the internal carotid artery; supplies blood to the temporal and parietal lobes of the cerebrum
middle sacral vein: drains the sacral region and leads to the left common iliac vein
occipital sinus: enlarged vein that drains the occipital region near the falx cerebelli and flows into the left and right transverse sinuses, and also into the vertebral veins
ophthalmic artery: branch of the internal carotid artery; supplies blood to the eyes
ovarian artery: branch of the abdominal aorta; supplies blood to the ovary, uterine (Fallopian) tube, and uterus
ovarian vein: drains the ovary; the right ovarian vein leads to the inferior vena cava and the left ovarian vein leads to the left renal vein
palmar arches: superficial and deep arches formed from anastomoses of the radial and ulnar arteries; supply blood to the hand and digital arteries
palmar venous arches: drain the hand and digits, and feed into the radial and ulnar veins
parietal branches: (also, somatic branches) group of arterial branches of the thoracic aorta; includes those that supply blood to the thoracic cavity, vertebral column, and the superior surface of the diaphragm
pericardial artery: branch of the thoracic aorta; supplies blood to the pericardium
petrosal sinus: enlarged vein that receives blood from the cavernous sinus and flows into the internal jugular vein
phrenic vein: drains the diaphragm; the right phrenic vein flows into the inferior vena cava and the left phrenic vein leads to the left renal vein
plantar arch: formed from the anastomosis of the dorsalis pedis artery and medial and plantar arteries; branches supply the distal portions of the foot and digits
plantar veins: drain the foot and lead to the plantar venous arch
plantar venous arch: formed from the plantar veins; leads to the anterior and posterior tibial veins through anastomoses
popliteal artery: continuation of the femoral artery posterior to the knee; branches into the anterior and posterior tibial arteries
popliteal vein: continuation of the femoral vein behind the knee; drains the region behind the knee and forms from the fusion of the fibular and anterior and posterior tibial veins
posterior cerebral artery: branch of the basilar artery that forms a portion of the posterior segment of the arterial circle; supplies blood to the posterior portion of the cerebrum and brain stem
posterior communicating artery: branch of the posterior cerebral artery that forms part of the posterior portion of the arterial circle; supplies blood to the brain
posterior tibial artery: branch from the popliteal artery that gives rise to the fibular or peroneal artery; supplies blood to the posterior tibial region
posterior tibial vein: forms from the dorsal venous arch; drains the area near the posterior surface of the tibia and leads to the popliteal vein
pulmonary artery: one of two branches, left and right, that divides off from the pulmonary trunk and leads to smaller arterioles and eventually to the pulmonary capillaries
pulmonary circuit: system of blood vessels that provide gas exchange via a network of arteries, veins, and capillaries that run from the heart, through the body, and back to the lungs
pulmonary trunk: single large vessel exiting the right ventricle that divides to form the right and left pulmonary arteries
pulmonary veins: two sets of paired vessels, one pair on each side, that are formed from the small venules leading away from the pulmonary capillaries that flow into the left atrium
radial artery: formed at the bifurcation of the brachial artery; parallels the radius; gives off smaller branches until it reaches the carpal region where it fuses with the ulnar artery to form the superficial and deep palmar arches; supplies blood to the lower arm and carpal region
radial vein: parallels the radius and radial artery; arises from the palmar venous arches and leads to the brachial vein
renal artery: branch of the abdominal aorta; supplies each kidney
renal vein: largest vein entering the inferior vena cava; drains the kidneys and leads to the inferior vena cava
right gastric artery: branch of the common hepatic artery; supplies blood to the stomach
sigmoid sinuses: enlarged veins that receive blood from the transverse sinuses; flow through the jugular foramen and into the internal jugular vein
small saphenous vein: located on the lateral surface of the leg; drains blood from the superficial regions of the lower leg and foot, and leads to the popliteal vein
splenic artery: branch of the celiac trunk; supplies blood to the spleen
straight sinus: enlarged vein that drains blood from the brain; receives most of the blood from the great cerebral vein and flows into the left or right transverse sinus
subclavian artery: right subclavian arises from the brachiocephalic artery, whereas the left subclavian artery arises from the aortic arch; gives rise to the internal thoracic, vertebral, and thyrocervical arteries; supplies blood to the arms, chest, shoulders, back, and central nervous system
subclavian vein: located deep in the thoracic cavity; becomes the axillary vein as it enters the axillary region; drains the axillary and smaller local veins near the scapular region; leads to the brachiocephalic vein
subscapular vein: drains blood from the subscapular region and leads to the axillary vein
superior mesenteric artery: branch of the abdominal aorta; supplies blood to the small intestine (duodenum, jejunum, and ileum), the pancreas, and a majority of the large intestine
superior phrenic artery: branch of the thoracic aorta; supplies blood to the superior surface of the diaphragm
superior sagittal sinus: enlarged vein located midsagittally between the meningeal and periosteal layers of the dura mater within the falx cerebri; receives most of the blood drained from the superior surface of the cerebrum and leads to the inferior jugular vein and the vertebral vein
superior vena cava: large systemic vein; drains blood from most areas superior to the diaphragm; empties into the right atrium
temporal vein: drains blood from the temporal region and leads to the external jugular vein
testicular artery: branch of the abdominal aorta; will ultimately travel outside the body cavity to the testes and form one component of the spermatic cord
testicular vein: drains the testes and forms part of the spermatic cord; the right testicular vein empties directly into the inferior vena cava and the left testicular vein empties into the left renal vein
thoracic aorta: portion of the descending aorta superior to the aortic hiatus
thyrocervical artery: arises from the subclavian artery; supplies blood to the thyroid, the cervical region, the upper back, and shoulder
transient ischemic attack (TIA): temporary loss of neurological function caused by a brief interruption in blood flow; also known as a mini-stroke
transverse sinuses: pair of enlarged veins near the lambdoid suture that drain the occipital, sagittal, and straight sinuses, and leads to the sigmoid sinuses
trunk: large vessel that gives rise to smaller vessels
ulnar artery: formed at the bifurcation of the brachial artery; parallels the ulna; gives off smaller branches until it reaches the carpal region where it fuses with the radial artery to form the superficial and deep palmar arches; supplies blood to the lower arm and carpal region
ulnar vein: parallels the ulna and ulnar artery; arises from the palmar venous arches and leads to the brachial vein
vertebral artery: arises from the subclavian artery and passes through the vertebral foramen through the foramen magnum to the brain; joins with the internal carotid artery to form the arterial circle; supplies blood to the brain and spinal cord
vertebral vein: arises from the base of the brain and the cervical region of the spinal cord; passes through the intervertebral foramina in the cervical vertebrae; drains smaller veins from the cranium, spinal cord, and vertebrae, and leads to the brachiocephalic vein; counterpart of the vertebral artery
visceral branches: branches of the descending aorta that supply blood to the viscera
- Anatomy & Physiology. Provided by : OpenStax CNX. Located at : http://cnx.org/contents/[email protected] . License : CC BY: Attribution . License Terms : Download for free at http://cnx.org/contents/[email protected]
- Read our Blog
- Media Gallery
- Become a Distributor
Telephone: +44 (0)118 921 2264

- Meet the Team
- History of Lorne
- Lorne Lab Service
- Career Opportunities
- Corporate Social Responsibilty
- Lorne Blood Grouping Reagents
- Enzymes, Potentiators & Accessories
- Blood Transfusion Equipment
- Millipore Blood Grouping Reagents
- Syphilis Kits
- Febrile Antigen Kits
- Biomixers & Biosealers
- Slide Stainer
- Temperature Monitors
- Rockland Immunochemicals
- Worthington Biochemicals
- Lorne Distributors
- Becoming an Export Customer
- Events & Exhibitions
- Technical Documents
- Contacting Lorne
The Journey of a Red Blood Cell
6 October 2017

Red Blood Cells (also known as Erythrocytes), are cellular components of blood. There are millions of them within the human body and their sole purpose is to carry oxygen from the lungs to tissues throughout the body, as well as carrying carbon dioxide to the lungs so it can be exhaled. The blood cell is characterised by a red colour due to the presence of hemoglobin, which is a protein that helps bind oxygen to the cell.
The red blood cell goes through a complex journey through the body, going from a deoxygenated blood cell to an oxygenated blood cell, and entering the heart twice. Below, we’ve laid out the journey of a red blood cell in the human body:
Step 1 - Creation of the Red Blood Cell
The journey starts with the red cell being created inside the bone. In the bone marrow, it develops in several stages starting as a hemocytoblast, then becoming an erythroblast after 2 to 5 days of development. After filling with hemoglobin it becomes a reticulocyte, which then becomes a fully matured red blood cell. This will be of a specific blood type, determined by the presence or absence of certain antibodies - learn more about blood grouping products here.
Step 2 - The Red Blood Cell's Journey begins
After creation, the red blood cell starts travelling to the heart via capillaries. The blood cell is currently deoxygenated.
Step 3 - Entering the Heart
The deoxygenated red blood cell now makes its way to the vena cava within the heart, and is then pushed into the right atrium.
The right atrium then contracts, pushing the blood cell through the tricuspid into the right ventricle.
The right ventricle then contracts, pushing the red blood cell out of the heart through the semi lunar.
Step 4 - Entering the Lungs and Oxygenation
After leaving the heart, the red blood cell travels through the pulmonary artery to the lungs. There it picks up oxygen making the deoxygenated red blood cell now an oxygenated blood cell. The blood cell then makes it way back to the heart via the pulmonary vein into the left atrium.
Step 5 - Re-entering the heart
After entering the left atrium, which then contracts and pushes the blood cell through the bicuspid, the red blood cell then enters the left ventricle.
The left ventricle then contracts, pushing the red blood cell through the semi lunar, and out of the heart into the aorta.
Step 6 - Travelling around the body
Travelling through the aorta, the red blood cell goes into the kidneys trunk and other lower limbs, delivering oxygenated blood around the body. They typically last for 120 days before they die.
And that’s the whole process! Although this seems like a lengthy process, the whole thing takes less than a minute from start to finish, depending on the individual’s heart rate.
In some cases such as illnesses or blood loss following injury or childbirth, the body may have too few red blood cells to provide the oxygen required by the body's extremities. This is where a blood transfusion becomes vital. At Lorne Laboratories all our blood grouping reagents and red cell products comply with the UK Red Book Standards to ensure safe blood transfusions.
Got questions about our products and how they impact the journey of the red blood cell? Email our team at Lorne Labs HQ and we'll be happy to assist you.


Yearly Archives
- All posts in 2014

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- Health Topics
- < Back To How the Heart Works
- How Blood Flows through the Heart
- What the Heart Looks Like
- How the Heart Beats
MORE INFORMATION
How the Heart Works How Blood Flows through the Heart
Language switcher.
Arteries and veins link your heart to the rest of the circulatory system. Veins bring blood to your heart. Arteries take blood away from your heart. Your heart valves help control the direction the blood flows.
Heart valves
Heart valves control the flow of blood so that it moves in the right direction. The valves prevent blood from flowing backward.
The heart has four valves.
- The tricuspid valve separates the right atrium and right ventricle.
- The mitral valve separates the left atrium and left ventricle.
- The pulmonary valve separates the right ventricle and the pulmonary artery.
- The aortic valve separates the left ventricle and aorta.
The valves open and shut in time with the pumping action of your heart's chambers. The opening and closing involve a set of flaps called cusps or leaflets. The cusps open to allow blood to flow out of a chamber and close to allow the chamber to refill with blood. Heart valve diseases can cause backflow or slow the flow of blood through the heart.
Learn about what the valves of the heart look like and do. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Adding oxygen to blood
Oxygen-poor blood from the body enters your heart through two large veins called the superior and inferior vena cava. The blood enters the heart's right atrium and is pumped to your right ventricle, which in turn pumps the blood to your lungs.
The pulmonary artery then carries the oxygen-poor blood from your heart to the lungs. Your lungs add oxygen to your blood. The oxygen-rich blood returns to your heart through the pulmonary veins. Visit our How the Lungs Work page to learn more about what happens to the blood in the lungs.
The oxygen-rich blood from the lungs then enters the left atrium and is pumped to the left ventricle. The left ventricle generates the high pressure needed to pump the blood to your whole body through your blood vessels.
When blood leaves the heart to go to the rest of the body, it travels through a large artery called the aorta. A balloon-like bulge, called an aortic aneurysm , can sometimes occur in the aorta.
Learn about how your heart circulates blood to your lungs and throughout your body. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Supplying oxygen to the heart’s muscle
Like other muscles in the body, your heart needs blood to get oxygen and nutrients. Your coronary arteries supply blood to your heart. These arteries branch off from the aorta so that oxygen-rich blood is delivered to your heart as well as the rest of your body.
- The left coronary artery delivers blood to the left side of your heart, including your left atrium and ventricle and the septum between the ventricles.
- The circumflex artery branches off from the left coronary artery to supply blood to part of the left ventricle.
- The left anterior descending artery also branches from the left coronary artery and provides blood to parts of both the right and left ventricles.
- The right coronary artery provides blood to the right atrium and parts of both ventricles.
- The marginal arteries branch from the right coronary artery and provide blood to the surface of the right atrium.
- The posterior descending artery also branches from the right coronary artery and provides blood to the bottom of both ventricles.
Your coronary arteries supply oxygen to your body. Medical Animation Copyright © 2022 Nucleus Medical Media, All rights reserved .
Some conditions can affect normal blood flow through these heart arteries. Examples include:
- Heart attack
- Coronary heart disease
The coronary veins return oxygen-low blood from the heart's muscles back to the right atrium so it can be pumped to the lungs. They include:
- The anterior cardiac veins
- The great cardiac vein
- The middle cardiac vein
- The small cardiac vein

- Literature & Fiction

Download the free Kindle app and start reading Kindle books instantly on your smartphone, tablet, or computer - no Kindle device required .
Read instantly on your browser with Kindle for Web.
Using your mobile phone camera - scan the code below and download the Kindle app.

Image Unavailable

- To view this video download Flash Player
Follow the authors

Journey Through Heartsongs Hardcover – January 21, 2002
Purchase options and add-ons.
- Print length 74 pages
- Language English
- Publisher Hyperion
- Publication date January 21, 2002
- Grade level 4 and up
- Reading age 18 years and up
- Dimensions 6.5 x 0.5 x 9.5 inches
- ISBN-10 9780786869428
- ISBN-13 978-0786869428
- See all details

Frequently bought together

Customers who bought this item also bought

Editorial Reviews
About the author, product details.
- ASIN : 0786869429
- Publisher : Hyperion; 1st edition (January 21, 2002)
- Language : English
- Hardcover : 74 pages
- ISBN-10 : 9780786869428
- ISBN-13 : 978-0786869428
- Reading age : 18 years and up
- Grade level : 4 and up
- Item Weight : 11.2 ounces
- Dimensions : 6.5 x 0.5 x 9.5 inches
- #29 in Poetry Writing Reference (Books)
- #1,315 in Inspirational & Religious Poetry (Books)
- #164,426 in Children's Books (Books)
About the authors
Mattie j. t. stepanek.
Mattie J.T. Stepanek was a poet, a peace activist, and the best-selling author of the Heartsongs poetry series. He was a motivational speaker and the National Goodwill Ambassador for the Muscular Dystrophy Association for three years. He died in June 2004 from dysautonomic mitochondrial myopathy. The Mattie Fund was established at MDA to specifically continue research of treatments and cures for childhood neuromuscular diseases.
Jennifer Smith Stepanek
Jeni Stepanek, Ph.D., is the mother of the late NY Times bestselling child poet and peacemaker, Mattie J.T. Stepanek, and the mother of three other children, Katie, Stevie, and Jamie, who also died due to a rare and fatal neuromuscular disease. Jeni was diagnosed with the adult onset form of the condition only after the births of all four of her children. Her son, Mattie, created six bestselling books of poetry, and one bestselling collection of peace essays. A published author or editor of numerous books, articles, and chapters, Jeni is also a noted and award-winning motivational speaker on topics ranging from disability and collaboration to bereavement and spirituality. She earned her doctoral degree in early childhood special education from the University of Maryland, College Park. Jeni, who relies on a power wheelchair for mobility and a ventilator for breathing support, serves as the Chair of the Mattie J.T. Stepanek Foundation, a National Vice President for the Muscular Dystrophy Association, and a Governor for the We Are Family Foundation. Her new book, "Messenger," is the first publication to offer the true story of her son's life, who "was as witty as he was wise." According to Jeni, "Messenger is not a sad story about a child's death, but an inspiring story of young man's life and his very real and ongoing message of hope and peace." She lives in Rockville, Maryland, near the 26 acre Mattie J.T. Stepanek Park and Peace Garden, and still travels with Mattie's service dog, Micah. When she grows up, Jeni wants to be a "beach chair philosopher."
For more information, visit www.mattieonline.com.
Customer reviews
Customer Reviews, including Product Star Ratings help customers to learn more about the product and decide whether it is the right product for them.
To calculate the overall star rating and percentage breakdown by star, we don’t use a simple average. Instead, our system considers things like how recent a review is and if the reviewer bought the item on Amazon. It also analyzed reviews to verify trustworthiness.
- Sort reviews by Top reviews Most recent Top reviews
Top reviews from the United States
There was a problem filtering reviews right now. please try again later..
Top reviews from other countries
- Amazon Newsletter
- About Amazon
- Accessibility
- Sustainability
- Press Center
- Investor Relations
- Amazon Devices
- Amazon Science
- Sell on Amazon
- Sell apps on Amazon
- Supply to Amazon
- Protect & Build Your Brand
- Become an Affiliate
- Become a Delivery Driver
- Start a Package Delivery Business
- Advertise Your Products
- Self-Publish with Us
- Become an Amazon Hub Partner
- › See More Ways to Make Money
- Amazon Visa
- Amazon Store Card
- Amazon Secured Card
- Amazon Business Card
- Shop with Points
- Credit Card Marketplace
- Reload Your Balance
- Amazon Currency Converter
- Your Account
- Your Orders
- Shipping Rates & Policies
- Amazon Prime
- Returns & Replacements
- Manage Your Content and Devices
- Recalls and Product Safety Alerts
- Conditions of Use
- Privacy Notice
- Consumer Health Data Privacy Disclosure
- Your Ads Privacy Choices
- Culture & Politics
- Diet & Nutrition
- Inspiration
- Pets and Animals
- Relationships
- Safety Tips
- Green Living
- Home Improvement
Norman Chapman, a name that may not ring a bell to many, but to those who are well-versed in the world of percussion, he is a legend. As an unsung hero of the drumming community, Chapman’s contributions to the art form are undeniable. From his early days in the music scene to his rise to prominence as a sought-after session player, Chapman’s story is one that deserves to be told. In this article, we will delve into the life and legacy of Norman Chapman, exploring his impact on the world of drumming and the lasting impression he has left on the music industry.
Table of Contents
- Unveiling the Legacy of Norman Chapman
- Exploring the Impact of Chapman’s Work on Modern Art
- Norman Chapman: A Pioneer in Abstract Expressionism
- Recommendations for Appreciating Chapman’s Artistry Today
- To Wrap It Up
Unveiling the Legacy of Norman Chapman
When one thinks of influential figures in the world of art and design, Norman Chapman may not be the first name that comes to mind. However, his contributions to the field have left a lasting impact that is still felt today. Known for his innovative and forward-thinking approach, Chapman’s work pushed the boundaries of traditional design and paved the way for future generations of artists.
- Chapman’s early work in the 1950s was marked by his unique use of color and form. He was not afraid to experiment with different mediums and techniques, resulting in a body of work that was both diverse and cohesive.
- His later work in the 1970s and 1980s saw a shift towards more minimalist designs, with a focus on functionality and simplicity. Despite this change in style, Chapman’s work remained distinctly his own, with a strong emphasis on craftsmanship and attention to detail.
In addition to his contributions to the world of art and design, Chapman was also a respected educator. He taught at several prestigious institutions, including the Rhode Island School of Design and the Art Institute of Chicago . His teachings have influenced countless artists and designers, many of whom have gone on to achieve great success in their own right.
Chapman’s legacy continues to inspire and influence the art and design world. His work is a reminder that creativity knows no bounds, and that true innovation comes from breaking away from the expected and embracing the unknown.
Exploring the Impact of Chapman’s Work on Modern Art
Norman Chapman’s work is often seen as a bridge between the traditional and the contemporary, blending classical techniques with modern themes. His influence on the art world can be seen in numerous ways, from the way he approached color and form, to his innovative use of materials. Chapman’s work challenged the norms of his time, pushing the boundaries of what was considered acceptable in the art world.
One of the most significant impacts of Chapman’s work is his exploration of the human form. He was known for his bold and expressive use of line, creating dynamic and powerful figures that resonated with viewers. Chapman’s work also often included elements of abstraction, blending realism with more conceptual ideas. This approach has inspired many contemporary artists, who have taken Chapman’s ideas and expanded on them in their own work.
- Use of vibrant and bold colors
- Innovative approach to mixed media
- Exploration of social and political themes
Chapman’s legacy can also be seen in the way he approached the role of the artist in society. He was known for his activism and used his art as a platform to address social and political issues. This has encouraged many modern artists to use their work as a means of sparking conversation and effecting change. Chapman’s work continues to be an important influence in the art world, inspiring artists to push the limits of what is possible.
Norman Chapman: A Pioneer in Abstract Expressionism
Norman Chapman was a trailblazer in the world of abstract expressionism. His bold use of color, texture, and form set him apart from his contemporaries and established him as a leader in the movement. His innovative techniques and fearless experimentation with new materials pushed the boundaries of what was considered “acceptable” in the art world.
Chapman’s early work was heavily influenced by the likes of Jackson Pollock and Willem de Kooning, but he quickly developed his own unique style. His large-scale canvases were filled with dynamic, gestural brushstrokes and a vibrant palette that captured the energy and emotion of the post-war era.
- Inspired by jazz music, Chapman often painted to the sounds of bebop and hard bop, infusing his work with a sense of rhythm and movement.
- He was also known for his use of non-traditional materials, such as sand and broken glass, which added texture and depth to his pieces.
- Despite facing criticism from more traditional art critics, Chapman remained steadfast in his vision and continued to push the limits of abstract expressionism.
Chapman’s impact on the art world cannot be understated. His influence can be seen in the work of countless artists who followed in his footsteps, and his paintings continue to be celebrated in galleries and museums around the world.
Through his work, Norman Chapman challenged viewers to see beyond the traditional boundaries of art and to find beauty in the chaos and complexity of the abstract world.
Recommendations for Appreciating Chapman’s Artistry Today
Norman Chapman’s artistry is a treasure that deserves to be appreciated by art enthusiasts and casual observers alike. To fully experience the depth and beauty of his work, there are several recommendations that can enhance your appreciation.
Firstly, take the time to study the details of his pieces. Chapman’s attention to detail is exquisite, and the more you look, the more you’ll find. Notice the intricate brushstrokes, the subtle use of color, and the way he captures light and shadow.
Another way to appreciate Chapman’s artistry is to understand the context in which it was created. Research the historical and cultural influences that shaped his work, and consider how these factors are reflected in his art. This will give you a deeper appreciation for the significance of his pieces.
Here are some additional recommendations for appreciating Chapman’s artistry:
– Visit galleries and museums that showcase his work to see it in person – Attend lectures or discussions about his art to gain insights from experts – Participate in art workshops that focus on his techniques and style
By following these recommendations, you can fully immerse yourself in the world of Norman Chapman and gain a greater appreciation for his remarkable artistry.
Q: Who is Norman Chapman? A: Norman Chapman is a renowned author and lecturer known for his expertise in economics and public policy.
Q: What is Norman Chapman’s background in economics? A: Chapman holds a PhD in economics from Harvard University and has published numerous scholarly articles and books on economic theory and public policy.
Q: What are some of Norman Chapman’s most notable works ? A: Chapman’s book “Economics in the Modern World” is widely regarded as a seminal work in the field of economics. He has also authored several influential papers on topics such as income inequality and economic development.
Q: What are some of the key themes that Norman Chapman explores in his writing? A: Chapman’s work often delves into the intersection of economics and social welfare, examining the impact of economic policies on issues such as poverty, education, and healthcare.
Q: In addition to his writing, what other activities is Norman Chapman involved in? A: In addition to his writing and research, Chapman is also a sought-after speaker and lecturer, and has served as a consultant for various government agencies and non-profit organizations.
Q: What is Norman Chapman’s approach to teaching and education? A: Chapman is known for his engaging and accessible teaching style, and is committed to making complex economic concepts understandable and relevant to a wide audience.
Q: What is the significance of Norman Chapman’s work in the field of economics? A: Chapman’s work has had a significant impact on the study and practice of economics, shaping the way we understand and address critical social and economic issues.
To Wrap It Up
In conclusion, Norman Chapman’s impact on the field of economics and his dedication to education and research are undeniable. His innovative ideas and passion for the subject have left a lasting impression on the academic community. As he continues to inspire and influence future generations of economists, it is clear that Norman Chapman’s contributions will be felt for years to come.
The Life of Katey Sagal: A Journey Through Heart Surgery
Katey Sagal has been captivating audiences for decades with her talent and charisma, but behind the glamorous facade of Hollywood lies a story of resilience and strength. Best known for her iconic roles in hit TV shows like “Married with Children” and “Sons of Anarchy,” Sagal has faced her fair share of challenges, including a major health scare that sent shockwaves through her fanbase. In this article, we will take a closer look at Katey Sagal’s heart surgery, shedding light on the woman behind the camera and her remarkable journey towards recovery.
- Early Career in Entertainment
- Family History of Heart Conditions
- Discovery of Heart Condition
- Decision to undergo surgery
- Recovery and Career Comeback
- Advocacy for Heart Health Awareness
- In Conclusion
Early Career in Entertainment
Katey sagal’s heart surgery.
Katey Sagal, best known for her roles in iconic TV shows like “Married… with Children” and “Sons of Anarchy,” has also had her fair share of health challenges throughout her career. In 2004, Sagal was diagnosed with a rare condition called arrhythmia, which led to her undergoing an emergency heart surgery. This health scare not only impacted her personal life but also her .
Despite facing such a critical medical condition , Katey Sagal showed immense resilience and determination to overcome her health issues. Her recovery from the heart surgery was a testament to her strength and passion for her craft. During this trying time, Sagal’s took a temporary halt as she focused on her health and well-being. However, her unwavering spirit and talent eventually led her back to the spotlight, where she continued to flourish as a versatile actress and singer.
Family History of Heart Conditions
Katey Sagal, the talented actress known for her roles in popular television shows like “Married… with Children” and “Sons of Anarchy,” has been open about her family’s history with heart conditions. Sagal’s mother, Sara Zwilling, passed away at the age of 78 due to heart disease. This tragic loss has had a significant impact on Sagal and her approach to her own heart health.
Following her mother’s passing, Sagal has been proactive in taking care of her heart. She has emphasized the importance of regular check-ups, maintaining a healthy lifestyle, and being aware of any symptoms that could indicate potential heart issues. Sagal’s dedication to her heart health serves as an inspiration to many, especially those with a .
Discovery of Heart Condition
Katey Sagal, the beloved actress known for her roles in popular TV shows like Sons of Anarchy and Married… with Children, recently made headlines after the shocking discovery of her heart condition. Sagal, who has been a prominent figure in the entertainment industry for decades, has always been known for her vibrant personality and unwavering spirit. However, her health took a frightening turn when she was diagnosed with a life-threatening heart condition that required immediate attention.
After experiencing symptoms such as fatigue and dizziness, Sagal underwent a series of medical tests that ultimately led to the discovery of a heart irregularity. The news came as a shock to the actress and her fans alike, and it was announced that she would need to undergo emergency heart surgery to address the condition. Despite the daunting prospect of such a major procedure, Sagal approached the situation with her trademark resilience, determined to overcome the health setback and emerge stronger than ever.
Sagal’s journey through the discovery of her heart condition serves as a powerful reminder of the importance of prioritizing health and well-being, even in the midst of a thriving career. Her unwavering determination and courage in the face of adversity continue to inspire fans and admirers around the world, and her successful recovery from the surgery has become a testament to the strength of the human spirit. As she continues to share her story, Sagal has become an advocate for heart health awareness, using her platform to raise awareness and encourage others to prioritize their cardiovascular well-being.
Decision to undergo surgery
After experiencing health issues, beloved actress Katey Sagal recently made the decision to undergo heart surgery. The decision was not taken lightly, as Sagal had been dealing with the effects of a heart arrhythmia for some time. After consulting with her doctors and considering her options, she ultimately chose to undergo the surgery in the hopes of improving her overall health and well-being.
For Sagal, the decision to undergo heart surgery was a deeply personal one. The actress, known for her roles in television shows such as “Married… with Children” and “Sons of Anarchy,” has always been candid about her health struggles. Through her openness and honesty, she has inspired countless fans to prioritize their own well-being and seek the necessary medical care. Sagal’s serves as a reminder of the importance of taking proactive steps to address health concerns, no matter how daunting they may seem.
Recovery and Career Comeback
After undergoing an unexpected heart surgery, Katey Sagal is making a remarkable recovery and gearing up for an inspiring career comeback. The beloved actress and singer, best known for her iconic roles in ”Married… with Children,” “Sons of Anarchy,” and “Futurama,” recently shocked fans with the news of her health scare. Sagal’s surgery, which took place earlier this year, was successfully completed, and she is now focused on regaining her strength and returning to the spotlight.
Despite the challenges posed by her health journey, Sagal remains determined to make a triumphant return to the entertainment industry. With her signature talent and unwavering resilience, she is set to captivate audiences once again with her exceptional performances. Fans and colleagues alike are eagerly anticipating her comeback, and Sagal’s unwavering spirit serves as an inspiration to all who have faced health setbacks.
Advocacy for Heart Health Awareness
It came as a shock to many fans when actress Katey Sagal revealed that she had undergone heart surgery. The beloved star, known for her roles in iconic TV shows such as Married… with Children and Sons of Anarchy, opened up about her health journey and emphasized the importance of heart health awareness. Sagal’s advocacy for heart health has resonated with fans and has sparked conversations about the prevalence of heart-related issues.
As someone who has been in the public eye for decades, Sagal’s decision to share her personal health struggles has brought about a renewed focus on the significance of regular check-ups and early detection. Her courage in speaking openly about her experience has encouraged many to prioritize their heart health and take proactive steps to prevent potential heart-related complications. Through her advocacy, Sagal has become a symbol of strength and resilience, using her platform to raise awareness and educate others about the importance of maintaining a healthy heart.
Q: Who is Katey Sagal? A: Katey Sagal is a well-known American actress and singer, best known for her roles in television shows like “Married… with Children,” “Sons of Anarchy,” and “Futurama.”
Q: Why was Katey Sagal in the news recently? A: Katey Sagal was in the news recently because she underwent heart surgery.
Q: When did Katey Sagal have heart surgery? A: Katey Sagal had heart surgery in 2021.
Q: What was the reason for Katey Sagal’s heart surgery? A: Katey Sagal underwent heart surgery to repair a “bowed out” aortic valve.
Q: How is Katey Sagal doing after her heart surgery? A: Katey Sagal is reportedly doing well and is on the road to recovery after her heart surgery.
Q: How did Katey Sagal’s fans react to the news of her heart surgery? A: Katey Sagal’s fans were concerned but supportive, sending her well wishes and prayers for a speedy recovery.
Q: Has Katey Sagal spoken about her experience with heart surgery? A: Katey Sagal has not spoken publicly about her experience with heart surgery, but her representatives have confirmed the successful outcome of the procedure.
Q: Will Katey Sagal’s heart surgery affect her career? A: It is not expected that Katey Sagal’s heart surgery will have a significant impact on her career, as she is expected to make a full recovery.
In Conclusion
As Katey Sagal continues on her road to recovery, she has shown incredible strength and resilience in the face of adversity. Her passion for life and dedication to her career and loved ones has only grown stronger through this experience. We wish her a speedy and full recovery, and look forward to seeing her back on the screen doing what she loves most. Sagal’s journey is a reminder of the importance of taking care of our health and the power of perseverance in the face of challenges. We stand in awe of her courage and send our love and support as she continues to heal.
Subscribe to our magazine
━ more like this, exploring the possibility of staying in cinderella’s castle, a comparative analysis of bellagio and caesars as luxury resorts, unleashing adrenaline: exploring extreme sports, exploring the depths: how deep can you go scuba diving, master the art of getting up on a wakeboard, unleashing the speed: exploring the world of bmx racers, unlock the thrills of nitroextreme: a guide to high-octane adventure, uncovering the ownership of kent watersports, leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.
Welcome to our complete News Portal about living, lifestyle, fashion and wellness. Take your time and immerse yourself in this amazing experience!
- Privacy Policy
- Contact Us / Advertising
- Terms and Conditions
━ follow us
━ subscribe.
© ThisWeekInLibraries All rights reserved.
- our america
Formerly unhoused and fighting to be her authentic self, Kaleef Starks put herself through college

"No one really believed in me in my home life at all. Education to me was sort of an escape honestly," said Kaleef Starks, a USC Annenberg Journalism M.S. Student.
"Being a black trans woman, being someone who experienced homelessness. I've been through a lot. My journey was something that it required a lot of patience. You know, I've always been attracted to radio and television."
"I grew up watching Barbara Walters, I grew up watching Oprah. I grew up in Fresno, California. So, I grew up to a working class family, I had a single father."
"A person like me is not typically accepted, any one of the LGBTQ communities, but especially a trans person. So, growing up, it was really hard. I went through a lot of bullying from people at school and in my home life as well."
"My parents were not accepting of me. And at 14, my father put me out in 2007 had nowhere to go. I was couch hopping with various family members. And they all had an issue with my identity literally everywhere I went. They were just like, you can't stay here. We don't we don't accept who you are."
"So, I decided to come here with my mom and my mom was homeless. She was living in a garage, living out of her car. She really didn't have much. It was a really toxic environment. I ran away several times. For me it was sort of like, oh, you know, I'm going to school. What more do you want? My mom really had a tough time finding employment. You know, which is why you know, we she was living in the garage at first and it wound up living in her car. Then we moved on to a shelter because it was so hard financially."
Angela M. Sanchez, a friend of Kaleef, stated, "We first met when we were both experiencing homelessness in a family shelter when I saw to leave him and I was like, Hi, can we be friends and so we actually had like our bunks next to each other. When we were both in the shelter Kaleef was definitely that spark of optimism, that sense of joy that liveliness that even though we're both homeless with our families, there was something that I looked forward to about having to have this experience with her. For both of us, we were each other's support, buddy while we were there. And later, I would go to UCLA. And then two years later, I would see Kaleef over at UCLA as well."
Kaleef continued, "I wound up getting into UCLA, and like my path just kind of changed. It didn't transition early, you know, some trans people transition early. I didn't have the ability to do that. But I already knew that I was a woman or a girl or whatever. I just didn't have the resources or the support to do that. It wasn't until I saw Isis King on America's Next Top Model. And when I saw her on the show, I was like, oh, like I was just like, oh, okay, you can transition. I didn't know that you could actually medically transition. I started around 18 as far as medically, but socially, I was already like, literally, dressing how I wanted to dress."
"After finishing UCLA and you know, getting my degree in gender studies and LGBTQ studies. I took some years off and I worked I worked at the Covenant House, California. And then I moved on to LA Children's Hospital, where I was a prep navigator, a sexual health counselor, and then I moved on. So, the Los Angeles LGBT Center where I worked for the National Institute against LGBTQ intimate partner violence. But I really loved education. I believed in education."
"Fun fact, I actually started an application to Annenberg in high school, but I chickened out, because I didn't believe in myself, I just did not believe that I would get in I did not think that I would be here. I applied and got accepted, and got offered the full ride scholarship with Wallace Annenberg, which was an honor to have, I'm the fourth person in America to have that. And you know, without that, I wouldn't be here for sure."
Heather John Fogarty, a former professor of Kaleef, mentioned, "The class where Kaleef and I collaborated, students were put into groups to work on projects, multimedia projects, and she just immediately distinguished herself as a leader."
Kaleef added, "I took advantage of the resources and I just use them to the best of my ability. So that's why you know, we have 'The Stark Effect.'"
"My recent podcast is called 'The Stark Effect.' I wanted it to feel like a daytime-ish energy. I was so lucky enough to find student producers here who believed in in the show and sometimes me being who I am it will make people uncomfortable. So that's something that I've had to navigate in the newsroom. I would like to be a part of that wave where you have a trans female journalist who's also an African American person where you know who they are, but it doesn't affect their careers."
Fogarty added, "My hope for Kaleef is that she has the opportunity to write her own story."
"I think the younger me is so proud. Although it's really hard and it's tough, the younger me and even both the mature me now, you know because in a lot of ways I've had to be my own parent but I think I'm really proud," stated Kaleef.
Sanchez continued, "I'm very proud of her and all the effort and work that she's put into this I know how hard this has been for her to achieve. And so I couldn't be happier for Kaleef and I'm going to be there for her on graduation day as well."
Related Topics
- RACE & CULTURE
- LGBTQ PRIDE
- LGBTQ+ PRIDE
- U.S. & WORLD
- OUR AMERICA SHOW WHO I'M MEANT TO BE 2024
- WHO I'M MEANT TO BE

Our America: Who I'm Meant to Be 2022 | Full Episode

Our America: Who I'm Meant to Be 2021 | Full Episode
Our america.

Our America: Who I'm Meant To Be 2024 | Full Episode

Our America: A Queen's Journey | Watch the full episode

What is Women's History Month, and why do we celebrate it?

Our America: Mission Montford Point | Watch the Full Episode
Top stories.

Ship in Lake Superior collides with something underwater: Coast Guard

Pro-Palestinian protest held at Buckingham Fountain
- 30 minutes ago

Man charged with killing his 2 brothers, setting mother's home on fire

Chicago Red Stars host historic soccer match at Wrigley Field
- 17 minutes ago

Pedestrian fatally struck by vehicle in south suburbs: police
Puerto Rican People's Parade held in Chicago
- 13 minutes ago
Woman killed in north suburban I-294 crash ID'd by medical examiner
- 2 hours ago
Man found guilty in 2019 murder of ex-girlfriend, mother of 6
- 32 minutes ago
Welcome to "Evidence Uncovered" where we discuss bothe solved, unsolved, and ongoing true crime cases. Join us on a gripping journey through the heart-pounding world of true crime and the intricate web of legal battles that follow. I'm your host Nicole and would love to hear from you. Are there any cases you want me to uncover? Reach out to [email protected].
Evidence Uncovered: True Crime and Legal Battles Evidence Uncovered
- MAY 25, 2024
Unraveling the Karen Read Case: An Introduction for Newcomers
Welcome to the first episode of "Evidence Uncovered: True Crime and Legal Battles"! In this episode, we delve into the intriguing Karen Read case, providing a comprehensive introduction for those who are unfamiliar with the details. We'll explore the background, key events, and major developments in the case, shedding light on the complexities and controversies surrounding it. Join us as we unravel the facts, discuss the implications, and set the stage for a deeper investigation into one of the most current talked-about cases displayed all over media. Whether you're a seasoned true crime enthusiast or new to the genre, this episode offers a thorough overview to get you up to speed.
- © Evidence Uncovered
Top Podcasts In True Crime
- Skip to main content
- Keyboard shortcuts for audio player
TED Radio Hour
- Subscribe to Breaking News Alerts

AsiaVision/Getty Images hide caption
Pain Relief: New approaches to how we live with pain
Thirty years into the opioid crisis, we still struggle to find other options for pain relief. This hour, TED speakers explain new understandings of how the brain interprets pain and new ideas to cope.

Courtesy of TED hide caption
An equestrian was crushed by her horse. How she's surviving with chronic pain
by Manoush Zomorodi , Rachel Faulkner White , Sanaz Meshkinpour

Jason Redmond / TED hide caption
Have we been misled about pain? How new understandings can help us better manage it
by Manoush Zomorodi , Matthew Cloutier , Sanaz Meshkinpour

Courtesy of Cammie Wolf Rice hide caption
How one mom is fighting the opioid crisis by asking hospitals to provide pain coaches
by Manoush Zomorodi , Fiona Geiran , Chloee Weiner , Sanaz Meshkinpour
- See TED Radio Hour sponsors and promo codes

NFL News: Green Bay Packers' Reunion with Eric Wilson Sparks Fan Enthusiasm, Bolsters Defense for 2024 Season
I n a move that has sent waves of excitement through the heartland of Wisconsin, Eric Wilson, the Green Bay Packers have once again demonstrated their knack for keeping the team spirit alive by re-signing linebacker Eric Wilson.
This decision, amid an offseason of tough calls, underscores the Green Bay Packers’ commitment to valuing heart and effort just as much as talent and stats. Eric Wilson’s journey from undrafted free agent to a cherished member of the Packers highlights the franchise’s keen eye for players who bring more to the table than just their on-field prowess.
A Testament to Tenacity, Eric Wilson’s Impactful Journey
The story of Eric Wilson is one of unwavering determination and sheer effort. Eric Wilson, whose career began undrafted in 2017, has carved a niche for himself in the NFL through grit and perseverance. His tenure with the Packers, although not marked by headline-grabbing stats, has been defined by moments that embody the spirit of football.
Perhaps no play better encapsulates Wilson’s importance to Green Bay than his crucial fumble recovery during the Divisional Round against the San Francisco 49ers—a play that showcased not only his athleticism but his acute game awareness.
Eric Wilson’s re-signing with the Packers for the 2024 season isn’t just a win for him but a statement by the team. In a league where the business aspect often overshadows loyalty, Green Bay ‘s move to keep Wilson is a refreshing reminder of the value of the human element in sports.
His performance, especially on special teams where he led with 308 snaps in the 2023 season, underscores the importance of roles that often go unnoticed but are critical to a team’s success.
Green Bay Packers Offseason Balances Change, Tradition
The Green Bay Packers’ offseason has been a rollercoaster, with significant changes that have both excited and worried fans. The departure of Aaron Jones, described by General Manager Brian Gutekunst as “the heartbeat of the team,” left many wondering about the direction of the franchise.
However, the acquisition of Josh Jacobs and the decision to retain Wilson, along with other key players, signals a strategic, albeit emotional, approach to team building. It’s a balance of embracing the new while honoring the contributions of players like Eric Wilson, who may not always be in the spotlight but whose presence is felt in every game.
Eric Wilson’s journey and subsequent retention are emblematic of the Packers’ philosophy—recognizing and rewarding the unsung heroes of the gridiron. His story is one of resilience, a testament to the fact that in football, as in life, effort and determination can take you far.
The linebacker’s return is celebrated not just in the locker room, with teammates like Rashan Gary showing their support with cheese emojis, but across the fan base, which appreciates the hard work and dedication Wilson brings to the team.
Green Bay Packers Re-Sign Eric Wilson, Solidify Core
As the Green Bay Packers gear up for the 2024 season, the re-signing of Eric Wilson, along with cornerback Keisean Nixon and tight end Tyler Davis, sets a positive tone for the team’s direction. These moves reflect a commitment to maintaining a core group of players who embody the Packers’ spirit and ethos.
Eric Wilson’s return is particularly noteworthy, highlighting the team’s appreciation for players who contribute significantly both on and off the field.
The story of Eric Wilson is far from over in Green Bay. As the team prepares for the challenges ahead, his presence serves as a reminder of what makes football so compelling—the blend of skill, heart, and an unyielding drive to succeed. For the Packers and their fans, Wilson’s re-signing is more than just a contract; it’s a celebration of the values that define the storied franchise.
Sources: ESPN
![In a move that has sent waves of excitement through the heartland of Wisconsin, Eric Wilson, the Green Bay Packers have once again demonstrated their knack for keeping the team spirit alive by re-signing linebacker Eric Wilson. This decision, amid an offseason of tough calls, underscores the Green Bay Packers’ commitment to valuing heart and effort just as much as talent and stats. Eric Wilson’s journey from undrafted free agent to a cherished member of the Packers highlights the franchise’s keen eye for players who bring more to the table than just their on-field prowess. A Testament to Tenacity, Eric […] In a move that has sent waves of excitement through the heartland of Wisconsin, Eric Wilson, the Green Bay Packers have once again demonstrated their knack for keeping the team spirit alive by re-signing linebacker Eric Wilson. This decision, amid an offseason of tough calls, underscores the Green Bay Packers’ commitment to valuing heart and effort just as much as talent and stats. Eric Wilson’s journey from undrafted free agent to a cherished member of the Packers highlights the franchise’s keen eye for players who bring more to the table than just their on-field prowess. A Testament to Tenacity, Eric […]](https://img-s-msn-com.akamaized.net/tenant/amp/entityid/BB1kv2W9.img?w=768&h=432&m=6&x=304&y=126&s=248&d=248)

IMAGES
VIDEO
COMMENTS
Join the Amoeba Sisters in their introduction to the circulatory system and follow the pathway of blood as it travels through the heart! This video explains ...
Blood flows through your heart, lungs and body in a series of steps. After delivering oxygen and nutrients to all your organs and tissues, your blood enters your heart and flows to your lungs to gain oxygen and get rid of waste. It then flows back to your heart, which pumps the refreshed blood out through your aorta to nourish your body again.
We've learned about the structure and function of the heart, but what does it really look like in there? What would it be like to be a red blood cell, and sw...
Animation of blood flow through the heart. How the heart works. The cycle of blood flow and the role of heart valves described. An updated version of this vi...
Pathway of Blood Through the Heart. In this educational lesson, we learn about the blood flow order through the human heart in 14 easy steps, from the superior and inferior vena cava to the atria and ventricles.Come also learn with us the heart's anatomy, including where deoxygenated and oxygenated blood flow, in the superior vena cava, inferior vena cava, atrium, ventricle, aorta, pulmonary ...
Blood then returns to the heart through the veins (vayns) and the cycle begins again. The Body's Superhighway Heart. Welcome to the hardest working muscle in your body. Your heart powers the circulatory system. Think of your heart as two pumps, working side by side. One pump receives oxygen-poor blood from your body and pushes it next door to ...
The heart is a unidirectional pump. Valves are present to prevent the backflow of blood. This unidirectional flow of blood through the heart shows that mammals have a double circulatory system ...
Oxygenated blood from the left side of the heart gets pumped out of the aorta. From there, blood flows through arteries, arterioles, and then capillaries (tiny blood vessels that transport blood, nutrients, and oxygen to cells). Deoxygenated blood from the capillaries then flows back to the heart through venules, veins, and ultimately through ...
All these pathways come together at the heart, the central pump through which all blood flows. This is a red blood cell, and it has an appointment to keep. The true workhorse of the bloodstream, this red blood cell is specifically designed to carry more oxygen faster than any mere fluid. There are 25 million million red blood cells.
After reaching their final destination, red blood cells need to make their way back to the heart and lungs. But the journey back to the heart is much slower than the fast-paced trip via the aorta. ... All blood from the veins enters the heart through the inferior or superior vena cava. Blood traveling from the lower body is directed to the ...
pulmonary circuit: system of blood vessels that provide gas exchange via a network of arteries, veins, and capillaries that run from the heart, through the body, and back to the lungs. pulmonary trunk: single large vessel exiting the right ventricle that divides to form the right and left pulmonary arteries.
The heart is an amazing organ. It starts beating about 22 days after conception and continuously pumps oxygenated red blood cells and nutrient-rich blood and other compounds like platelets throughout your body to sustain the life of your organs.; Its pumping power also pushes blood through organs like the lungs to remove waste products like CO2.; This fist-sized powerhouse beats (expands and ...
The red blood cell goes through a complex journey through the body, going from a deoxygenated blood cell to an oxygenated blood cell, and entering the heart twice. Below, we've laid out the journey of a red blood cell in the human body: Step 1 - Creation of the Red Blood Cell. The journey starts with the red cell being created inside the bone.
Adding oxygen to blood. Oxygen-poor blood from the body enters your heart through two large veins called the superior and inferior vena cava. The blood enters the heart's right atrium and is pumped to your right ventricle, which in turn pumps the blood to your lungs. The pulmonary artery then carries the oxygen-poor blood from your heart to the ...
The Journey Through My Heart- Is a collection of poetry and prose, on topics of self-love, friendships, relationships, love, death and grieving, and toxicity. Anyone seeking to find themselves, and for positive affirmations, this book is for you. Genres PoetryLove. 184 pages, Paperback. Published April 19, 2018.
"The Journey Through My Heart" is a captivating collection of poetry and prose that delves into the depths of human emotions and experiences. Within its pages, readers will embark on a transformative journey encompassing a wide range of themes, including self-love, friendships, relationships, love, death and grieving, and toxicity.
Unveil the Hidden Secrets of Your Heart: Dive into its Chambers, Valves, and Blood Flow! Join us in this captivating exploration of the human heart's remarka...
One of the first things you will notice if you look at the 12 steps is the pattern between the right and left side of the heart is similar. Step 1 and 6 involve a blood vessel, which makes sense as this is how blood enters and exits that side of the heart. Steps 2-5 involve a chamber, valve, chamber, and valve.
Hardcover - January 21, 2002. Mattie J.T. Stepanek takes us on a Journey Through Heartsongs with more of his moving poems. These poems share the rare wisdom that Mattie has acquired through his struggle with a rare form of muscular dystrophy and the death of his three siblings from the same disease. His life view is one of love and generosity ...
Sagal's journey through the discovery of her heart condition serves as a powerful reminder of the importance of prioritizing health and well-being, even in the midst of a thriving career. Her unwavering determination and courage in the face of adversity continue to inspire fans and admirers around the world, and ...
Lampe had multiple, serious congenital heart defects, including a non-working aortic valve, aortic stenosis - or narrowing of the aortic valve that prevents healthy blood flow - and a hole between her two heart chambers. Jeremiah also had a narrow aorta known as coarctation of the aorta but his condition wasn't as complex as his mother's.
It is a journey through what I call the "Three Planes," a personal philosophy I've developed centered around the idea that we each travel through three realms of reality each and every day ...
At 26, Finley Survives the Unthinkable, Thanks to Bystander CPR Knowledge and AED Usage. Toward the end of a race last year, the heart rhythm of Philadelphia resident Victoria Finley took a perilous detour. At the age of 26, Victoria collapsed from cardiac arrest just after completing mile 7 of the run. However, fate intervened in the form of vigilant bystanders who quickly initiated life ...
This talk was given at a local TEDx event, produced independently of the TED Conferences. What is love indeed?Born to parents from two different continents, ...
"No one really believed in me in my home life at all. Education to me was sort of an escape honestly," said Kaleef Starks, a USC Annenberg Journalism M.S. Student. "Being a black trans woman ...
Evidence Uncovered: True Crime and Legal Battles on Apple Podcasts. 1 episode. Welcome to "Evidence Uncovered" where we discuss bothe solved, unsolved, and ongoing true crime cases. Join us on a gripping journey through the heart-pounding world of true crime and the intricate web of legal battles that follow. I'm your host Nicole and would love ...
Thirty years into the opioid crisis, we still struggle to find other options for pain relief. This hour, TED speakers explain new understandings of how the brain interprets pain and new ideas to cope.
Artist: Final RequestTitle: A Journey Through The HeartLabel: AtlantRelease date: October 14, 2022Beatport/Spotify:http://li.sten.to/ATL066
This decision, amid an offseason of tough calls, underscores the Green Bay Packers' commitment to valuing heart and effort just as much as talent and stats. Eric Wilson's journey from ...